Abstract
Objective: US military veterans are at elevated risk for suicide. High levels of suicide-specific cognitions, an indicator of chronic suicide risk, have been found to predict suicidal behaviors. The objective of this study was to examine data from a large, nationally representative sample of US veterans to determine the prevalence and correlates of high chronic suicide risk, with the goal of providing population-level insight into veterans who may be most at risk.
Methods: This study utilized data from the 2019–2022 National Health and Resilience in Veterans Study, a nationally representative sample (N = 2,430), to determine the prevalence of veterans who screened positive for high chronic risk for suicide based on the Brief Suicide Cognitions Scale. The relative importance of sociodemographic, military, health, and psychosocial characteristics associated with high chronic risk was also examined.
Results: In total, 250 veterans screened positive for high chronic suicide risk. Analyses revealed that veterans at high risk were lower educated and more likely to report suicidal ideation and disability in activities of daily living. They also endorsed a higher number of adverse childhood experiences and scored lower on measures of protective psychosocial characteristics and social connectedness. Relative importance analyses revealed that lower levels of perceived resilience, social support, and purpose in life accounted for the majority of the explained variance in high chronic suicide risk.
Conclusions: Results suggest that interventions to bolster these positive psychological traits may help reduce suicide risk and death by suicide in veterans.
Prim Care Companion CNS Disord 2025;27(1):24m03821
Author affiliations are listed at the end of this article.
Suicide is a public health crisis and a leading cause of death in US military veterans.1 Veterans continue to die by suicide at higher rates than their nonveteran counterparts.1 For example, in 2021, despite accounting for less than 6% of the total population, veterans accounted for approximately 13% of all suicide deaths in the United States.1 In spite of ongoing efforts to reduce veteran suicide,2 considerable work is still needed to identify factors that may potentiate or mitigate suicide risk in this vulnerable population.
The difficulty in predicting suicide attempts and deaths is partly due to their complex etiology. Both theoretical and empirical research support the notion that suicide risk varies as a function of biological, psychological, and sociocultural factors that can be either enduring or time limited in nature.3,4 For example, the fluid-vulnerability theory (FVT)5 proposes that there are individual differences in chronic, or long-term, risk for suicidal thoughts and behaviors, which affect acute risk—the likelihood that a person will engage in suicidal behavior during times of heightened stress or crisis (eg, the period following sudden job loss). Chronic suicide risk is influenced by numerous factors, including genetic makeup and formative early life experiences.5
Suicide-specific cognitions, including beliefs about the self as unlovable, emotional experiences as unbearable, and life problems as unsolvable, are often operationalized as an important indicator of chronic suicide risk.5 Research indicates suicide-specific cognitions are better predictors of incident suicidal behaviors than traditional indicators, such as suicidal ideation or psychiatric symptoms.6 For instance, Bryan and colleagues7 showed that, in a large sample of military and civilian adults seen in primary care, higher scores on the Suicide Cognitions Scale-Revised (sample item: “No one is as loathsome as me”),8 but not suicidal ideation or depressive symptom severity, distinguished those who attempted suicide from those who only thought about suicide 1 year later.
Strong endorsement of suicide-specific conditions may be one reason why US veterans continue to die by suicide at such startling rates.1 Veterans commonly endorse experiences associated with suicide-specific cognitions, including adverse childhood experiences and combat exposure,9 which are linked to increased vulnerability to stress and emotion dysregulation.10,11 They also endorse high rates of disorders, such as alcohol use disorder,12 which could potentiate suicide risk during periods of acute stress, especially in the presence of other risk factors.13 Nevertheless, no known studies have examined the prevalence and correlates of suicide specific cognitions in a population-based sample of US military veterans. Accordingly, in the current study, we analyzed data from a large, nationally representative sample of US veterans to examine the prevalence and correlates of the Brief Suicide Cognitions Scale (B-SCS),5 with the goal of providing population-level insight into veterans who may be at high chronic risk of suicide.
METHODS
Sample
A total of 2,430 veterans participated in the 2019–2022 National Health and Resilience in Veterans Study, which surveyed a nationally representative sample of US military veterans. The sample was ascertained from KnowledgePanel, a survey panel of more than 50,000 US households maintained by Ipsos, a research firm. KnowledgePanel is a probability-based survey panel of a representative sample of US adults that covers approximately 98% of US households. To permit generalizability of results to the US veteran population, poststratification weights using benchmark distributions of US military veterans from the 2019 Veterans Supplement of the US Census Bureau Current Population Survey were applied. In the current study, all independent variables were assessed during a Wave 1 survey conducted in the fall/winter of 2019–2020. Suicide-specific cognitions were assessed as part of a 3-year follow-up survey conducted in the fall of 2022. Additional details about the methodology can be found in the Supplementary Material.
Measures
Suicide-specific cognitions. Suicide-specific cognitions were assessed using the 6-item B-SCS, a self-report measure that assesses maladaptive beliefs, such as those related to the lovability of the self. Responses range from (1) strongly disagree to (5) strongly agree. The 6 items are as follows: (1) I am completely unworthy of love, (2) nothing can help me solve my problems, (3) I can’t cope with my problems any longer, (4) I can’t imagine anyone being able to withstand this kind of pain, (5) there is nothing redeeming about me, and (6) suicide is the only way to end this pain. The Cronbach alpha in the current study was 0.90. Based on previous research showing that a score ≥13 on the B-SCS accurately predicted future suicidal behavior (eg, attempts; sensitivity: 1.00),5 and considering the B-SCS scores were severely zero-inflated, we operationalized a total score ≥13 as indicative of clinically significant chronic risk for suicide.
A broad range of sociodemographic (ie, age, sex, race/ ethnicity, education, marital status, and household income), military (ie, combat exposure and military sexual trauma), psychiatric (ie, adverse childhood experiences; cumulative trauma burden; frequency of nonsuicidal self-injury; positive screens for current posttraumatic stress disorder, major depressive disorder, generalized anxiety disorder, alcohol use disorder, and drug use disorder; current suicidal ideation; lifetime history of suicide attempt; and loneliness); physical health (ie, total number of medical conditions, presence of disability in activities of daily living [ADL]); and protective characteristics (ie, positive psychosocial characteristics [composite score of perceived resilience, purpose in life, gratitude, optimism, curiosity, grit, and perceived community integration] and social connectedness [composite score of structural social support, perceived social support, and attachment style]) were examined as correlates of high suicide risk as measured using the B-SCS. Supplementary Table 1 provides a description of these measures.
Data Analysis
Data analyses proceeded in 4 steps. First, descriptive statistics were computed to estimate the prevalence of veterans who scored below or ≥13 on the B-SCS. Second, weighted independent samples t tests and χ2 analyses were conducted to compare veterans who were and were not considered to be at greater chronic risk for suicide, based on the B-SCS, on sociodemographic, military, psychiatric, physical health, and protective characteristics. Third, a multivariable binary logistic regression analysis was conducted to examine the association between the aforementioned correlates and B-SCS screening status. Only variables that differentiated veterans with low or high suicide-specific cognitions based on the ≥13 B-SCS cut score at the P < .01 level in bivariate analyses were included in this analysis. Fourth, planned post hoc analyses of composite variables that emerged as significant correlates were conducted to identify specific variables linked to suicide risk. Fifth, a relative importance analysis14 was conducted to determine the relative contribution of each significant correlate to the model-explained variance (ie, R2).
RESULTS
On average, participants (N = 2,430) were 63.2 years old (SD = 14.0; range = 22–96). Most were male (N = 2,173; weighted 92.1%) and non-Hispanic white (N = 2,024; 79.6%). The remainder were non-Hispanic black (N = 164; 10.2%), Hispanic (N = 163; 6.0%), or biracial/multiracial and other groups (N = 79; 4.3%).
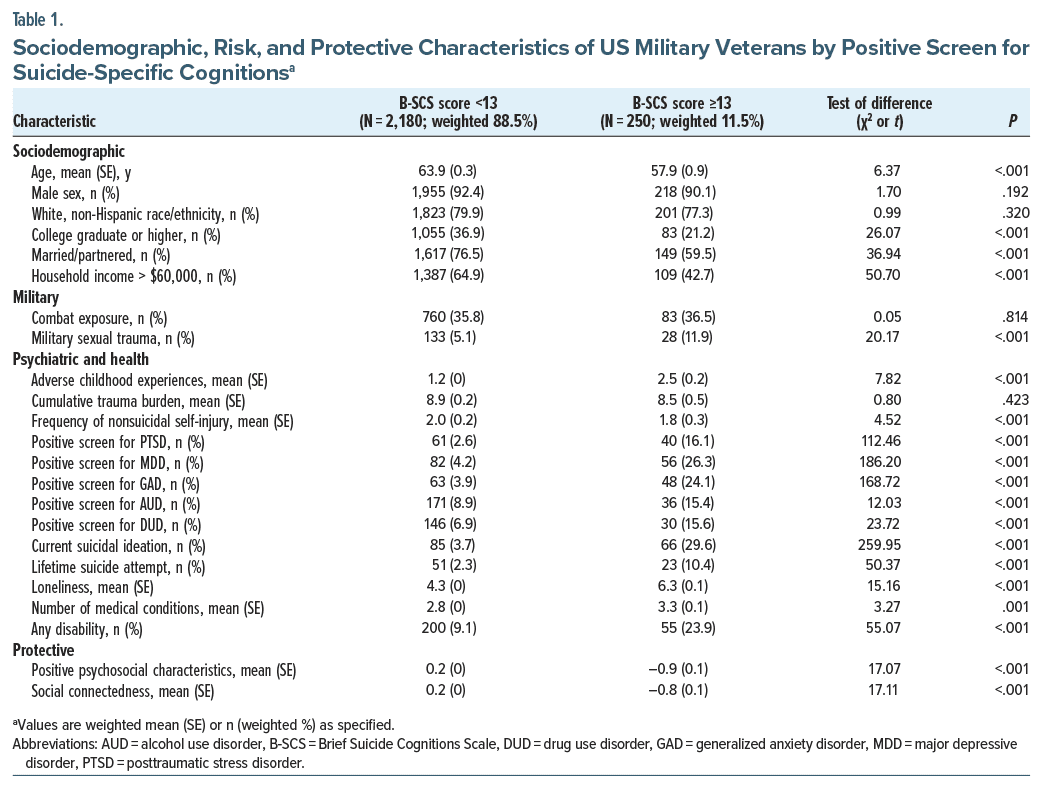
In the total sample, 250 veterans (weighted 11.5%) scored ≥13 on the B-SCS, indicating strong endorsement of suicide-specific cognitions and potentially elevated chronic risk for suicide.5 Table 1 provides an overview of sample characteristics by B-SCS screening status.
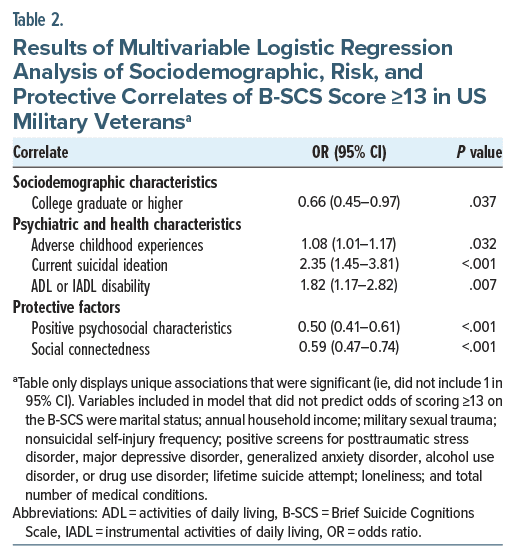
Table 2 shows results of a multivariable binary logistic regression analysis examining independent correlates of B-SCS screening status (see footnote a for full details). Results indicated that, relative to veterans who scored below 13 on the B-SCS and considered at low chronic risk for suicide, veterans who scored ≥13 on the B-SCS were less likely to have a college degree or higher education and more likely to endorse current suicidal ideation and the presence of an ADL or instrumental ADL (IADL) disability. They also endorsed a greater number of adverse childhood experiences and scored lower on measures of positive psychosocial characteristics and social connectedness.
Planned post hoc analyses revealed that lower levels of perceived resilience (odds ratio [OR] = 0.95; 95% CI, 0.89–0.98), purpose in life (OR = 0.94; 95% CI, 0.91–0.97), and gratitude (OR = 0.81; 95% CI, 0.71–0.92) were independently associated with B-SCS screening status. Post hoc analyses further revealed that lower levels of perceived social support (OR = 0.93; 95% CI, 0.90–0.97) and structural social support (OR = 0.95; 95% CI, 0.91–0.99) were independently associated with B-SCS screening status.
A relative importance analysis revealed that the majority of variance explained in the model predicting B-SCS screening status (Nagelkerke R2 = 0.34) was accounted for by lower levels of perceived resilience (23.7% relative variance explained [RVE]), lower perceived social support (19.3% RVE), and lower purpose in life (19.3%). Lower gratitude (11.0%), endorsement of current suicidal ideation (8.9%), lower structural social support (8.4%), higher number of adverse childhood experiences (3.7%), the presence of ADL/IADL disability (3.0%), and lower education (2.7%) explained the remainder of the variance.
DISCUSSION
The present study, to our knowledge, is the first to examine the prevalence and correlates of the B-SCS,5 one indicator of chronic risk for suicide, in a nationally representative sample of US military veterans. Research indicates that suicide-specific beliefs and schemas, such as those measured by the B-SCS, may have a better prognostic utility in predicting suicidal behavior than traditional approaches to assessing suicide risk (eg, suicidal ideation).6 Moreover, given the vast majority of questions on the B-SCS do not specifically reference suicide, it offers the potential to circumvent questions that require direct endorsement of suicidal ideation,15 which may be under-endorsed due to stigma or perceived negative consequences.16 This is important given that nearly half of individuals who die by suicide deny having suicidal ideation during their most recent health care appointment.17,18 Thus, establishing the prevalence and correlates of suicide-specific cognitions in a vulnerable population may help advance suicide prevention efforts.
We found that 11.5% of the sample scored ≥13 on the B-SCS, which corresponds to the clinical cutoff score established in a prior psychometric investigation to identify individuals at elevated risk for prospective suicide attempts.5 Understood within the context of the FVT,5 these results suggest that approximately 1 in 10 US military veterans may be at significantly elevated chronic suicide risk due, in part, to maladaptive beliefs about the self as unlovable, one’s emotional experience as unbearable, and life’s problems as unsolvable.5 Consistent with prior work,19 suicidal ideation and depressive symptoms were only modestly associated with the B-SCS, suggesting these constructs are related but distinct.
Perceived resilience, as measured by the Connor Davidson Resilience Scale (CD-RISC),20 emerged as the strongest correlate of suicide cognitions. The CD-RISC measures various aspects of perceived resilience, defined as characteristics that enable an individual to adapt and thrive in the face of adversity.20 This finding resonates with prior work,21,22 which has observed a strong relationship between perceived psychological resilience and suicide risk among veterans. For example, a longitudinal study of US Iraq and Afghanistan war veterans found a protective effect of higher CD-RISC scores (eg, greater resilience) on suicidal ideation and attempts.22 It is plausible that lower levels of perceived resilience can predispose veterans to the development of maladaptive suicide-related beliefs.5 Conversely, it is also possible that higher levels of suicide-specific beliefs and schemas contribute to lower perceptions of resilience. Moreover, considering the apparent similarity between certain items on the CD-RISC and the B-SCS (eg, sample CD-RISC item: “I can deal with whatever comes my way”; sample B-SCS item: “I can’t cope with my problems any longer”), the manifest association may also be measurement related. Longitudinal research is needed to examine the temporal relationships between these constructs and the mechanisms that may underlie the association.
Lower social support and purpose in life emerged as the strongest correlates of suicide-specific cognitions after perceived resilience. These findings align with prior research showing that both social support and purpose in life play an important role in modulating risk for the engagement in suicidal behavior among veterans.23 For example, a recent population-based prospective cohort study found that lower purpose in life and perceived social support were the strongest predictors of incident suicidal ideation and attempts among veterans over a 10-year period.24 This study also found that lower levels of these protective factors were more strongly associated with suicidal behaviors than traditional risk factors, such as psychiatric disorders and history of suicide attempt. Collectively, the current results parallel other recent findings, which suggest that veterans who endorse low levels of specific adaptive psychosocial characteristics (eg, purpose in life, resilience, social support) may be a subgroup who are at particularly high risk for suicidal behavior.25 Consequently, considering the profound negative effect that experiences of loneliness and lack of purpose can also have on health more generally,26,27 efforts to promote purpose in life and social connection may be crucial to both suicide prevention and the promotion of overall health and well-being in US military veterans.
The current findings should be considered within the context of 3 limitations. First, this study was based on cross-sectional data, which precludes temporal or causal interpretation of the observed associations. Further research employing prospective designs is needed to examine the temporal relationships and mechanisms that underlie these associations. Second, the current sample was limited to veterans, the majority of whom are older, male, and of white ethnicity. Thus, while our results may be representative of the general US veteran population, further research is needed to evaluate whether the current findings generalize to other veteran subgroups, such as female and racial/ethnic-minority veterans, or active-duty military who are much more diverse.28 Finally, although we employed a cut score that has been shown to identify individuals at high risk for suicidal behavior,5 suicide risk exists on a continuum, and individuals considered low risk based on the cut score may still be vulnerable and should be monitored appropriately.
Despite these limitations, the current findings have several implications. As noted, accumulating research suggests that suicide-specific cognitions may yield valuable incremental utility for predicting suicidal behaviors relative to more traditional risk indices, such as suicidal ideation.6 Results of this study indicated that lower levels of 3 protective factors—perceived resilience, social support, and purpose in life—accounted for the majority of the explained variance in suicide-specific beliefs among a wide range of empirically derived risk variables (eg, adverse childhood experiences).23 Given that each of these protective factors have been shown to be modifiable,29–31 research is needed to clarify whether increases in these constructs reliably contribute to decreases in suicide-specific cognitions. For example, in active duty populations, there is preliminary evidence showing that improvements in purpose in life may be a mechanism of change in suicide-specific treatments32 and can protect against suicide over the course of a military deployment.33 Continued investigation into the role that protective factors, such as purpose in life and social connectedness, play in the development and amelioration of suicide-specific cognitions may help to advance knowledge about the most efficient targets for suicide prevention. Research that addresses whether particular cultural contexts affect the development or reduction of these protective factors may help to identify specific treatment targets. For example, there is some evidence showing that higher levels of unit cohesion34 and purpose in service33 can protect against the development of suicidal ideation. Continued research in this area may reveal that aspects of military culture are important mechanisms of suicide intervention and not just contextual factors to consider in treatment settings.
Article Information
Published Online: January 14, 2025. https://doi.org/10.4088/PCC.24m03821
© 2025 Physicians Postgraduate Press, Inc.
Submitted: July 26, 2024; accepted October 2, 2024.
To Cite: Fischer IC, Nichter B, Trachik B, et al. Resilience and vulnerability: suicide specific cognitions in a nationally representative sample of US military veterans. Prim Care Companion CNS Disord. 2025;27(1):24m03821.
Author Affiliations: US Department of Veterans Affairs National Center for Posttraumatic Stress Disorder, VA Connecticut Healthcare System, West Haven, Connecticut (Fischer, Pietrzak); Department of Psychiatry, Yale School of Medicine, New Haven, Connecticut (Nichter, Pietrzak); Behavioral and Policy Sciences Department, RAND, Santa Monica, California (Trachik); Department of Psychiatry and Behavioral Health, The Ohio State University College of Medicine, Columbus, Ohio (Bryan); Department of Social and Behavioral Sciences, Yale School of Public Health, New Haven, Connecticut (Pietrzak).
Corresponding Author: Ian C. Fischer, PhD, US Department of Veteran Affairs National Center for Posttraumatic Stress Disorder, VA Connecticut Healthcare System, 950 Campbell Ave, West Haven, CT 06516 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: Preparation of this manuscript was supported in part by the US Department of Veterans Affairs Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment.
Role of the Sponsor: The US Department of Veterans Affairs had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclaimer: Material has been reviewed by the Walter Reed Army Institute of Research. There is no objection to its presentation and/or publication. The opinions or assertions contained herein are the private views of the author and are not to be construed as official, or as reflecting true views of the Department of the Army or the Department of Defense. The investigators have adhered to the policies for protection of human subjects as prescribed in AR 70–25.
Supplementary Material: Available at Psychiatrist.com.
Clinical Points
- Assessment of suicide-specific cognitions may enhance the identification of individuals at high chronic risk of suicide.
- A total of 11.5% of US military veterans may be at high chronic risk for suicide based on the Brief Suicide Cognitions Scale.
- Interventions that promote social support and purpose in life may mitigate chronic suicide risk by reducing the severity of suicide-specific cognitions.
References (34)

- Affairs USDoV. 2023 National Veteran Suicide Prevention Annual Report. Secondary 2023 National Veteran Suicide Prevention Annual Report 2023. U.S. Department of Veterans Affairs; 2023.
- Rubin R. Task force to prevent veteran suicides. JAMA. 2019;322(4):295–95.
- Turecki G, Brent DA, Gunnell D, et al. Suicide and suicide risk. Nat Rev Dis Primers. 2019;5(1):74.
- Kleiman EM, Turner BJ, Fedor S, et al. Examination of real-time fluctuations in suicidal ideation and its risk factors: results from two ecological momentary assessment studies. J Abnorm Psychol. 2017;126(6):726–738.
- Rudd MD, Bryan CJ. The Brief Suicide Cognitions Scale: development and clinical application. Front Psychiatry. 2021;12:737393. PubMed
- Bryan CJ, Thomsen CJ, Bryan AO, et al. Scores on the Suicide Cognitions Scale-Revised (SCS-R) predict future suicide attempts among primary care patients denying suicide ideation and prior attempts. J Affect Disord. 2022;313:21–26. PubMed
- Bryan CJ, Rudd MD. Suicidal ideation and suicidal beliefs as prospective indicators of suicidal behavior among primary care patients. Psychiatry Res Commun. 2023;3(2):100107.
- Bryan CJ, May AM, Thomsen CJ, et al. Psychometric evaluation of the Suicide Cognitions Scale-Revised (SCS-R). Mil Psychol. 2022;34(3):269–279.
- Blosnich JR, Garfin DR, Maguen S, et al. Differences in childhood adversity, suicidal ideation, and suicide attempt among veterans and nonveterans. Am Psychol. 2021;76(2):284–299.
- Cloitre M, Khan C, Mackintosh M-A, et al. Emotion regulation mediates the relationship between ACES and physical and mental health. Psychol Trauma. 2019;11(1):82–89.
- Nichter B, Hill M, Norman S, et al. Associations of childhood abuse and combat exposure with suicidal ideation and suicide attempt in US military veterans: a nationally representative study. J Affect Disord. 2020;276:1102–1108. PubMed
- Fuehrlein BS, Kachadourian LK, DeVylder EK, et al. Trajectories of alcohol consumption in US military veterans: results from the national health and resilience in veterans study. Am J Addict. 2018;27(5):383–390.
- Lange S, Jiang H, Kaplan MS, et al. Association between acute alcohol use and firearm-involved suicide in the United States. JAMA Netw Open. 2023;6(3):e235248. PubMed
- Tonidandel S, LeBreton JM. Determining the relative importance of predictors in logistic regression: an extension of relative weight analysis. Organ Res Methods. 2010;13(4):767–781.
- Rudd MD, Bryan CJ. Finding effective and efficient ways to integrate research advances into the clinical suicide risk assessment interview. Front Psychiatry. 2022;13:846244. PubMed
- Sharp M-L, Fear NT, Rona RJ, et al. Stigma as a barrier to seeking health care among military personnel with mental health problems. Epidemiol Rev. 2015;37(1):144–162.
- Bryan CJ, Allen MH, Thomsen CJ, et al. Improving suicide risk screening to identify the highest risk patients: results from the PRImary care Screening Methods (PRISM) study. Ann Fam Med. 2021;19(6):492–498.
- Simpson SA, Goans C, Loh R, et al. Suicidal ideation is insensitive to suicide risk after emergency department discharge: performance characteristics of the Columbia-Suicide Severity Rating Scale Screener. Acad Emerg Med. 2021;28(6):621–629.
- Ellis TE, Rufino KA. A psychometric study of the Suicide Cognitions Scale with psychiatric inpatients. Psychol Assess. 2015;27(1):82–89.
- Connor KM, Davidson JR. Development of a new resilience scale: the Connor Davidson resilience scale (CD-RISC). Depress Anxiety. 2003;18(2):76–82.
- Roy A, Sarchiapone M, Carli V. Low resilience in suicide attempters. Arch Suicide Res. 2007;11(3):265–269.
- Youssef NA, Green KT, Beckham JC, et al. A 3-year longitudinal study examining the effect of resilience on suicidality in veterans. Ann Clin Psychiatry. 2013;25(1):59–66.
- Pietrzak RH, Pitts BL, Harpaz-Rotem I, et al. Factors protecting against the development of suicidal ideation in military veterans. World Psychiatry. 2017;16(3):326–327.
- Fischer IC, Nichter B, Feldman DB, et al. Purpose in life protects against the development of suicidal thoughts and behaviors in US veterans without a history of suicidality: a 10-year, nationally representative, longitudinal study. J Affect Disord. 2023;340:551–554. PubMed
- Nichter B, Stein MB, Monteith LL, et al. Risk factors for suicide attempts among US military veterans: a 7-year population-based, longitudinal cohort study. Suicide Life Threat Behav. 2022;52(2):303–316.
- Luo Y, Hawkley LC, Waite LJ, et al. Loneliness, health, and mortality in old age: a national longitudinal study. Soc Sci Med. 2012;74(6):907–914.
- Kim ES, Shiba K, Boehm JK, et al. Sense of purpose in life and five health behaviors in older adults. Prev Med. 2020;139:106172. PubMed
- Army US. Active Component Demographics. Secondary Active Component Demographics; 2022. https://api.army.mil/e2/c/downloads/2022/11/15/62a2d64b/active-component-demographic-report-october-2022.pdf
- Southwick SM, Pietrzak RH, White G. Interventions to enhance resilience and resilience-related constructs in adults. In: SouthwickSM, LitzBT, CharneyD, et al. eds. Resilience and Mental Health: Challenges Across the Lifespan. Cambride University Press; 2011:289–306.
- Manco N, Hamby S. A meta-analytic review of interventions that promote meaning in life. Am J Health Promot. 2021;35(6):866–873.
- Swinkels L, Hoeve M, Ter Harmsel J, et al. The effectiveness of social network interventions for psychiatric patients: a systematic review and meta-analysis. Clin Psychol Rev. 2023;104:102321. PubMed
- Bryan CJ, Bryan AO, Rozek DC, et al. Meaning in life drives reductions in suicide risk among acutely suicidal soldiers receiving a crisis response plan. J Soc Clin Psychol. 2019;38(9):774–787.
- Trachik B, Oakey-Frost N, Ganulin ML, et al. Military suicide prevention: the importance of leadership behaviors as an upstream suicide prevention target. Suicide Life Threat Behav. 2021;51(2):316–324.
- Trachik B, Moscardini EH, Ganulin ML, et al. Perceptions of purpose, cohesion, and military leadership: a path analysis of potential primary prevention targets to mitigate suicidal ideation. Mil Psychol. 2022;34(3):366–375.
Enjoy this premium PDF as part of your membership benefits!