Lessons Learned at the Interface of Medicine and Psychiatry
The Psychiatric Consultation Service at Massachusetts General Hospital sees medical and surgical inpatients with comorbid psychiatric symptoms and conditions. During their twice-weekly rounds, Dr Stern and other members of the Consultation Service discuss diagnosis and management of hospitalized patients with complex medical or surgical problems who also demonstrate psychiatric symptoms or conditions. These discussions have given rise to rounds reports that will prove useful for clinicians practicing at the interface of medicine and psychiatry.
Prim Care Companion CNS Disord 2024;26(5):24f03783
Author affiliations are listed at the end of this article.
Have you ever wondered what you should say to a patient who asks whether they should try a psychedelic? Have you been uncertain about the benefits and risks of psychedelics taken for medical or psychiatric conditions? Have you worried that it seems more patients, particularly those with depression, are using psychedelics?1 Have you been uncertain about the potential liability associated with discussing (or recommending) drugs not approved for use by the US Food and Drug Administration (FDA)? If you have, the following case vignette and discussion should prove useful.
CASE VIGNETTE
Ms A, an unmarried, unemployed, childless, 58-year old woman, lives an isolated existence; she has collected social security disability insurance for lower back pain for more than 30 years. Her medical history is notable for a body mass index of 37 kg/m2, and she has hypertension, hypercholesterolemia, mitral regurgitation, nonalcoholic steatohepatitis, obstructive sleep apnea, chronic headaches, and low back pain. Her surgical history includes 2 knee replacements more than a decade ago and coronary artery bypass grafting surgery nearly a decade ago. Her psychiatric history is remarkable for major depressive disorder (MDD), which led to numerous low-lethality suicide attempts and psychiatric hospitalizations in her 20s and 30s. She takes lisinopril, labetalol, atorvastatin, and Fioricet, as well as sertraline and an antipsychotic (for insomnia), which are prescribed by a psychiatric nurse practitioner every 6 months. Ms A’s father died from cardiac causes, and both her sister and maternal grandmother have bipolar disorder. She spends most of her day watching shows on her computer. Her physician is concerned that she remains depressed and that being overweight is putting her at increased risk for complications of obesity. At today’s appointment, she states that she watched a Netflix program about psychedelics. She did some research and found a group that offers ayahuasca retreats near her home. She asks if she should try ayahuasca.
WHAT ARE PSYCHEDELICS AND HOW DO THEY WORK?
Psychedelics are agents that elicit a potent change in consciousness that is often described as profound or meaningful. These experiences are frequently accompanied by the blurring of boundaries between one’s internal world and the external world (termed ego dissolution); this experience may be deeply positive, anxiety provoking, or terrifying.2 Psychedelics also produce heightened sensory experiences, typically with an enrichment of the sense of vision, visual patterns or hallucinations, and sometimes synesthesia (ie, experiencing one sense as another sense).2
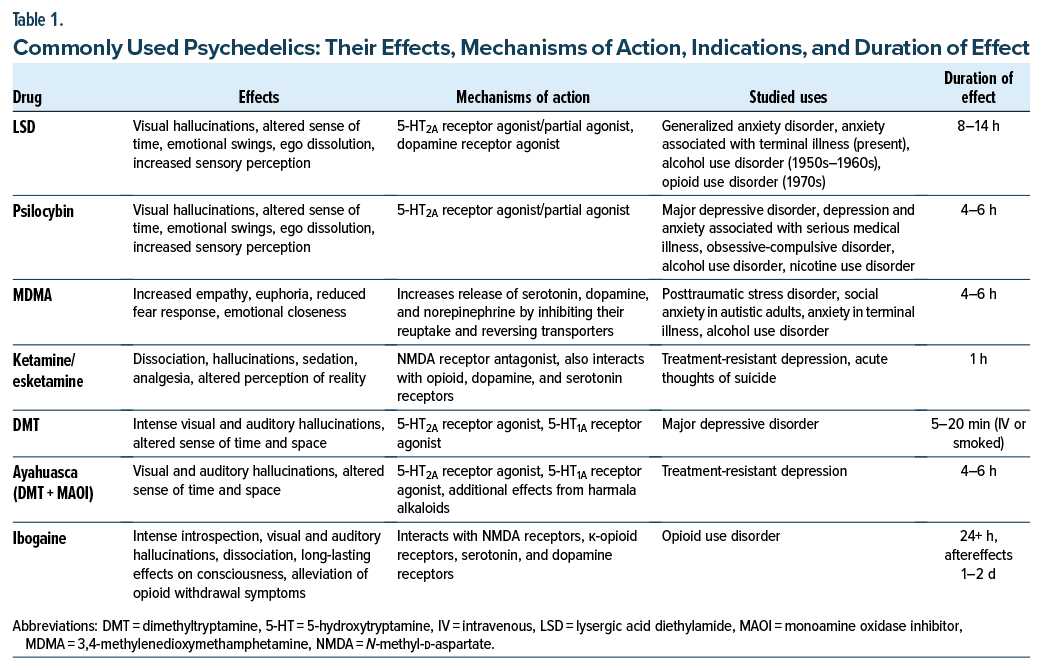
Drugs in this category include the classic psychedelics, such as psilocybin (that occurs naturally in many fungi), lysergic acid diethylamide (LSD, or “acid”), mescaline (found in peyote and in San Pedro cacti), and dimethyltryptamine (DMT). Of note, DMT, which occurs naturally in many plants worldwide, has no oral bioavailability due to the actions of monoamine oxidase (MAO), which rapidly degrades DMT in the gut. However, ayahuasca is a brew made of different plants that contain both DMT and alkaloids having MAO-inhibiting properties, which render the DMT orally active. In addition, atypical psychedelics include ibogaine (a psychedelic with effects that last longer than 24 hours) and ketamine (a dissociative anesthetic with psychedelic properties, which has been used to treat depression). 3,4-Methylenedioxymethamphetamine (MDMA) is classified as an empathogen due to its ability to produce feelings of warmth, empathy, and trust but is also often classified as a psychedelic.3
The classic psychedelics are partial agonists at the serotonin2A receptor4 that promote neuroplasticity, increasing the formation of synaptic proteins and dendritic spines.5 Neuroimaging studies conducted while subjects experience acute effects of psychedelics have shown reduced integrity within certain higher-order neural networks (such as the default mode network, which is associated with self-representation) and increased connectivity between brain networks that normally operate discretely.6 Current models propose that psychedelics loosen previously held self epresentations and beliefs while boosting receptivity to external sensory information and promoting the update of these beliefs during a period of heightened neuroplasticity.7 This may allow for the revision of repetitive narratives, thoughts, and behaviors associated with anxiety, depression, and posttraumatic stress disorder (PTSD).
HAVE PSYCHEDELICS BEEN STUDIED WIDELY IN CLINICAL SETTINGS?
Over the span of several decades, psychedelics have been administered in clinical trials in the presence of staff who have been trained to prepare participants for the experience, to navigate potential challenges, and to integrate and solidify any queries that have arisen. In clinical populations, this has typically been referred to as psychedelic-assisted therapy, although some models use more muted language such as “providing psychological support.” While disagreements persist in the field as to what the optimal nature and form of psychological assistance should involve when providing psychedelics to patients,8,9 no modern study has provided psychedelics in the absence of psychological support.10 For this reason, the term set and setting is often used to emphasize the importance of mindset as one prepares to take a psychedelic (which may require extensive psychological and emotional preparation), as well as a setting in which this is to occur (often looking more like a living room than a hospital room or clinic).11 In addition, psychedelics have been used clinically by special license for both individual and group psychotherapy in Switzerland since 2014,12 as well as in Australia since 2023.13 Considerable efforts are now underway to bring psychedelics to market as medicines worldwide.14
WHY HAS THE USE OF PSYCHEDELICS BEEN CONTROVERSIAL?
Many medical providers are unaware of the extensive research and clinical use of psychedelics in the 1950s and 1960s.15 During this era, thousands of patients were treated with LSD. Moreover, hundreds of clinical studies on psychedelics have been published. Most of those studies examined psychedelics’ effects as “psychotomimetics” (as a paradigm for schizophrenia, a model that fell out of favor by the late 1960s)4 and the impact of psychedelics on alcoholism. Unfortunately, the public’s perception of psychedelics shifted rapidly in the 1960s to one of negativity due to a “moral panic” over the use of LSD and its association with counterculture movements of the time.16 Paralleling the enactment of the Controlled Substances Act of 1971 (and the creation of its enforcement body, the US Drug Enforcement Administration), there were numerous “information” campaigns that claimed that psychedelics had adverse effects, ranging from increased incidences of cancer to genetic mutations, and that a variety of psychiatric conditions were due to illicit psychedelic use.
Unfortunately, while these campaigns solidified the public’s negative view toward psychedelics, they were not scientifically based. However, recent years have seen a considerable warming of psychiatrists’ attitudes toward psychedelics as treatments, with a striking increase in positive views found between 2016 and 2022.17
WHICH PSYCHIATRIC CONDITIONS HAVE IMPROVED FOLLOWING PSYCHEDELIC USE?
Phase 2 clinical trials have reported efficacy for psilocybin-assisted therapy for treatment-resistant depression (TRD),18 MDD,19 and alcohol use disorder (AUD)20 and for LSD in anxiety disorders.21 Phase 3 trials have reported efficacy for MDMA-assisted therapy in PTSD.22,23 The field suffered a setback on August 9, 2024, when the FDA rejected a new drug application for MDMA-assisted therapy, requesting an additional clinical trial. While this application had been for the treatment of PTSD, potential off-label uses include anxiety disorders,24 alcohol use,25 and adjunct to couples therapy.26 Numerous early-phase clinical trials and pilot studies have been conducted or are underway examining psychedelics for conditions such as obsessive-compulsive disorder,27 chronic pain,28 and irritable bowel syndrome.29 Although esketamine has been approved by the FDA for the treatment of depression, it is subject to a restrictive risk evaluation and mitigation strategy and is not generally delivered in the form of a psychedelic assisted therapy.30 However, evidence supports the efficacy of racemic ketamine for the acute reduction in depressive symptoms31 and thoughts of suicide,32 although the durability of these effects appears limited.31
WHAT ARE THE MEDICAL RISKS AND CONTRAINDICATIONS TO TAKING A PSYCHEDELIC?
Classic psychedelics, such as psilocybin and LSD, are generally thought to be medically safe, even when taken in high doses. Physiological effects typically include mild elevations in heart rate, blood pressure, and body temperature that lack clinical significance for most patients.33 MDMA and ketamine can each have more pronounced effects on blood pressure than classic psychedelics,34,35 although, for ketamine, these effects may be less clinically significant when subanesthetic doses are used (ie, for depression).36 In all cases, uncontrolled hypertension has been a contraindication in clinical trials, and it will likely remain so once psychedelics are approved for medical use. Repeated use of ketamine has been associated with interstitial cystitis, although this is rare when ketamine has been prescribed for depression.37 High doses of MDMA can cause serotonin syndrome,38 and in the setting of excessive physical activity and increased water consumption (such as occurs at dances or “raves”), it has induced hyponatremia, seizures, and death.39 Classic psychedelics (psilocybin, LSD) may also increase the risk of seizure in patients with a personal or family history of epilepsy.40 Due to potential impacts on driving abilities, in modern clinical trials of psychedelics, participants are told not to drive until the day after receiving a psychedelic.
Ibogaine has been linked to significant QT interval prolongation, which can result in serious arrhythmias such as Torsades de pointes.41 Cases of cardiac arrest or sudden death have been reported following the ingestion of ibogaine.42 This potential risk necessitates a thorough medical evaluation for individuals considering its use, and it should be completely avoided by those with preexisting heart conditions; recently, magnesium has been investigated to potentially mitigate this risk.43
Many substances, including psilocybin,44 LSD,45 and MDMA,46 are agonists of the serotonin2B receptor. This mechanism is shared by the drug fenfluramine, which was withdrawn from the market (as fenfluramine phentermine) due to causing serious valvular heart disease.47 While there is currently no clear evidence suggesting that any of these psychedelics could have a similar effect, the potential risk cannot be entirely dismissed, and further research is warranted.
Psilocybin, DMT, and LSD are predominantly metabolized by the liver, with inactive metabolites then renally excreted.48,49 The rates of metabolism and excretion vary greatly among the specific substances and are directly correlated with their duration of effect (Table 1). A careful review of the patient’s medication list is necessary, and caution should be exercised if it includes medications that may interfere with the metabolism of psychedelics, such as monoamine oxidase inhibitors (MAOIs).
WHAT PSYCHIATRIC RISKS HAVE BEEN ASSOCIATED WITH TAKING PSYCHEDELICS?
Although many adverse effects of psychedelics were reported in the 1960s and 1970s, these findings, originally based on poor science, have since been refuted. This includes the risk of chromosomal damage and an increased incidence of cancer in people who used psychedelics.50,51 Unfortunately, such claims continue to be cited. For example, a 2002 Science article claimed to show that recreational doses of MDMA produced severe neurotoxic effects in nonhuman primates; however, it was later retracted due to the revelation that the authors had utilized high-dose methamphetamine rather than MDMA.52,53
Nevertheless, psychedelics are not risk free. It is likely that individuals who cannot tolerate a higher cardiovascular load could be at risk for adverse cardiovascular effects from the classic psychedelics, as well as MDMA and ketamine. It is unclear how renal or hepatic impairment might contribute to adverse effects due to impaired metabolism or clearance. Psychiatric and behavioral risks and adverse events are of a greater general overall concern, particularly in settings in which use is for recreational purposes or is carried out outside of a controlled environment. Adequate preparation and setting are key to mitigating the adverse impact of challenging experiences if and when they occur. Challenging experiences can leave lasting impressions that negatively influence postpsychedelic well-being,54 and even in the absence of a negative experience, “ontological shock” (a rapid shift in worldview due to a powerful psychedelic experience) can leave individuals psychologically or existentially unmoored without proper supports in place.55 Unfortunately, isolated cases of patients becoming anxious or paranoid, attempting suicide, becoming agitated, or taking one’s life have been reported.56,57
Clinicians who work in emergency departments are probably familiar with patients who have been brought in with agitation or disorganized thinking due to ingestion of a psychedelic. While the overall risk of self-harm and harm to others is substantially lower for psychedelics than for more commonly abused substances (such as alcohol, cocaine, or methamphetamine),58 these events do occur. Due to the rapid induction of tachyphylaxis, the classic psychedelics have low potential for abuse4; however, both MDMA and ketamine have been shown to carry a risk of disordered use that is higher than that of classical psychedelics.59,60
An additional risk involves whether psychedelics can precipitate prolonged psychosis (eg, schizophrenia) or bipolar disorder. Since patients at risk for psychosis and mania have been excluded from modern clinical trials, this risk is largely theoretical and relies on older literature that used outdated diagnostic criteria, as well as case reports that lacked clarity on the actual drug consumed or occurred in the context of other drug use. Data from a population-level study of Swedish adolescent twins found no association between the onset of psychotic symptoms and psychedelic use after controlling for other drug use.61 A recent survey also found no association between psychedelic use during the study period and an increase in psychotic symptoms.62 However, the authors62 found an association between more frequent manic symptoms in individuals with either a personal or a family history of bipolar disorder who had used psychedelics during the study period. Lastly, a recent study of psilocybin with psychotherapy for bipolar II depression found no increases in hypomania, although the sample size was small and risks may be different for patients with type I bipolar disorder.63 While further information is needed to refine our understanding of these relationships, most experts now advise against psychedelic use in any individual with a history of mania or psychosis. In addition, a person with a primary relative with type 1 bipolar disorder or a psychotic disorder may also be at increased risk, particularly if the exposure occurred during the window of vulnerability generally associated with the onset of those conditions.
DO DRUG-DRUG INTERACTIONS ARISE WITH PSYCHEDELICS?
Serotonin reuptake–inhibiting drugs have been well known for their ability to attenuate the effects of psychedelics. While some survey data support this,64 recent studies appear to suggest that selective serotonin reuptake inhibitors (SSRIs) attenuate neither the subjective nor the therapeutic effects of psilocybin.65,66 However, the effects of MDMA have been almost completely prevented by the coadministration of SSRIs as well as serotonin-norepinephrine reuptake inhibitors.67 Fatalities have been reported in the setting of MDMA when combined with moclobemide, a reversible MAO inhibitor.68 While not a risk associated with psychedelics per se, an important potential interaction (as was present in Ms A) is with ayahuasca. As described previously, ayahuasca incorporates both DMT (the psychedelic agent) and an MAO inhibitor that renders DMT orally active. Therefore, serotonin syndrome could arise if ayahuasca is consumed with antidepressants such as SSRIs or tricyclic antidepressants. Patients should be cautioned about such interactions.
Adverse interactions may occur between lithium and classic psychedelics (eg, LSD and psilocybin). A study of interactions reported on psychedelic user forums found a substantial incidence in reports of seizures in those taking LSD or psilocybin while on lithium.69 Because of its QT prolonging effects, ibogaine is thought to carry an increased risk of inducing Torsades de pointes in the presence of other QT-prolonging drugs, including SSRIs, certain antibiotics, and methadone (given that most patients seeking ibogaine treatment do so for opioid use disorder).
Atypical antipsychotics and the research drug ketanserin—serotonin2A antagonists—have successfully aborted the acute effects of psychedelics.70 However, haloperidol, which primarily antagonizes dopamine receptors, may worsen certain aspects of a psychedelic experience, and thus, second-generation antipsychotics are a safer and more effective option in emergency settings.70
WHAT ARE THE LEGAL/LIABILITY CONCERNS, AND ARE PATIENT RESOURCES AVAILABLE?
Except for ketamine (and its S-enantiomer esketamine), no psychedelics are currently available as medical or psychiatric treatments anywhere in the United States, and they remain classified as DEA schedule 1 drugs, meaning they have no accepted medical use. Therefore, providing, recommending, or facilitating access to most psychedelics could result in legal and/or state licensing board disciplinary action. However, despite their illegality, savvy patients may be able to obtain various psychedelics, and given the increasing interest, the American Psychiatric Association recommends a harm reduction approach in certain circumstances with the caveat that harm reduction does not include violating the law.71
The general approach to a patient who expresses an interest in psychedelics such as psilocybin or MDMA should be to note that while studies are promising, these drugs are currently only available in research settings, and they do not yet have FDA-approved indications. If a patient attempted these treatments on their own, they might face risks, including legal exposure, risks regarding lack of drug purity or adulterants, psychological risks from unsupported or poorly supported underground facilitation, and in some cases medical risks. In addition, ketamine is currently available, both in the form of infusions without psychotherapy, as intranasal esketamine, and in the form of ketamine assisted psychotherapy (KAP). KAP practitioners can be located by searching on websites such as PsychologyToday.com. Patients can also be directed to ClinicalTrials.gov to see if there might be a trial near them for which they are eligible.
If a patient is going to seek out their own psychedelic experience, harm-reduction practices may include counseling about known specific medical and psychiatric risks to the patient, addressing potential drug-drug interactions (particularly in the case of ayahuasca given the presence of an MAOI), and referral to online resources for safe practices, including drug purity testing sites (Dancesafe.org, Rollsafe. org) and the psychedelic harm-reduction peer support network Fireside Project (Firesideproject.org). The Multidisciplinary Association for Psychedelic Studies has a resource page on psychedelic integration that may be useful for some patients for both education as well as other psychotherapeutic information and guidance.72 The Johns Hopkins Center for Psychedelic and Consciousness Research also has released a brief educational video on these issues that may be of use for patients.73
WHAT HAPPENED TO MS A?
Ms A’s history of cardiovascular disease and valvular disease suggested that she was at risk for adverse medical events from psychedelics. In addition, several other factors, such as the absence of a robust mental health care team or social network, indicated she would likely face a lack of support were she to experience any challenges in the aftermath of a psychedelic experience that did not occur in conjunction with regular mental health care. She also was prescribed psychiatric medications that would put her at risk of serotonin syndrome were she to ingest ayahuasca. Ultimately, after a dedicated effort by the office administrator, she was successfully connected to a therapist and a psychiatrist with whom she could meet more frequently than her previous prescriber. She was also started on semaglutide injections; after 8 months, her BMI decreased to 33 kg/m2. She was then referred to a therapist who specialized in KAP, who worked with her primary mental health care team and her internist and provided several KAP sessions. Over time, she tapered and discontinued 2 of her psychotropic medications, which led to and supported an ongoing effort at weight loss, which she has been able to maintain.
CONCLUSION
The last several years have seen a precipitous increase in both scientific publications and public interest in psychedelics (ie, agents that elicit a potent change in consciousness that is often described as profound or meaningful). Driven largely by glowing media reports of rapid and durable reductions in symptoms of a wide variety of conditions, interest has continued to grow among patients and mental health clinicians. While certain psychedelics are available in other countries, following a rejection of MDMA in August 2024, FDA approval of any nonketamine psychedelic is not expected to occur for another few years, producing a tension between public interest and safe and legal availability. As a result, clinicians should make a concerted effort to learn more about psychedelics (eg, how they work, what they might work for, and what their adverse effects encompass).
Article Information
Published Online: October 15, 2024. https://doi.org/10.4088/PCC.24f03783
© 2024 Physicians Postgraduate Press, Inc.
Submitted: May 31, 2024; accepted August 8, 2024.
To Cite: King F, Nahlawi A, Stern TA. Talking to your patients about psychedelics: using an informed approach and understanding indications, risks, and benefits. Prim Care Companion CNS Disord. 2024;26(5):24f03783.
Author Affiliations: Massachusetts General Hospital, Boston, Massachusetts (King, Nahlawi, Stern); Harvard Medical School, Boston, Massachusetts (King, Stern).
Corresponding Author: Franklin King IV, MD, Harvard Medical School, Massachusetts General Hospital, 55 Fruit St, WRN 606, Boston, MA 02114 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Clinical Points
- Current clinical trials have reported efficacy for psilocybin assisted therapy in treatment-resistant depression, major depressive disorder, and alcohol use disorder; for lysergic acid diethylamide (LSD) in anxiety disorders; and for 3,4- methylenedioxymethamphetamine-assisted therapy in posttraumatic stress disorder.
- Classic psychedelics, such as psilocybin and LSD, are generally thought to be medically safe even when taken in high doses; physiological effects typically include mild elevations in heart rate, blood pressure, and body temperature that lack clinical significance for most patients.
- Ayahuasca incorporates both dimethyltryptamine (DMT) (the psychedelic agent) and a monoamine oxidase inhibitor that renders DMT orally active; therefore, serotonin syndrome may arise if ayahuasca were to be consumed with antidepressants such as selective serotonin reuptake inhibitors or tricyclic antidepressants.
References (73)

- Walsh CA, Gorfinkel L, Shmulewitz D, et al. Use of lysergic acid diethylamide by major depression status. JAMA Psychiatry. 2024;81(1):89–96. PubMed
- Preller KH, Vollenweider FX. Phenomenology, structure, and dynamic of psychedelic states. Curr Top Behav Neurosci. 2018;36:221–256. PubMed CrossRef
- Vollenweider FX, Liechti ME, Gamma A, et al. Acute psychological and neurophysiological effects of MDMA in humans. J Psychoactive Drugs. 2002;34(2):171–184. PubMed CrossRef
- Nichols DE. Psychedelics. Pharmacol Rev. 2016;68(2):264–355. PubMed
- Ly C, Greb AC, Cameron LP, et al. Psychedelics promote structural and functional neural plasticity. Cell Rep. 2018;23(11):3170–3182. PubMed CrossRef
- Carhart-Harris RL, Leech R, Erritzoe D, et al. Functional connectivity measures after psilocybin inform a novel hypothesis of early psychosis. Schizophr Bull. 2013;39(6):1343–1351. PubMed CrossRef
- Carhart-Harris RL, Friston KJ. Rebus and the anarchic brain: toward a unified model of the brain action of psychedelics. Pharmacol Rev. 2019;71(3):316–344. PubMed CrossRef
- Goodwin GM, Malievskaia E, Fonzo GA, et al. Must psilocybin always “assist psychotherapy”? Am J Psychiatry. 2024;181:20–25. PubMed
- Schenberg EE, King F IV, da Fonseca JE, et al. Is poorly assisted psilocybin treatment an increasing risk? Am J Psychiatry. 2024;181(1):75–76.
- Carhart-Harris RL, Roseman L, Haijen E, et al. Psychedelics and the essential importance of context. J Psychopharmacol. 2018;32(7):725–731. PubMed CrossRef
- Noorani T. Containment matters: set and setting in contemporary psychedelic psychiatry. Philosophy, Psychiatry Psychol. 2021;28(3):201–216.
- Oehen P, Gasser P. Using a MDMA- and LSD-group therapy model in clinical practice in Switzerland and highlighting the treatment of trauma-related disorders. Front Psychiatry. 2022;13:863552. PubMed CrossRef
- Therapeutic Goods Administration. Canberra A, ed. Notice of final decisions to amend (or not amend) the current poisons standard in relation to psilocybine and MDMA. Department of Health, Commonwealth of Australia; 2023.
- Aday JS, Barnett BS, Grossman D, et al. Psychedelic commercialization: a wide spanning overview of the emerging psychedelic industry. Psychedelic Med. 2023;1(3):150–165.
- Hall W. Why was early therapeutic research on psychedelic drugs abandoned? Psychol Med. 2022;52(1):26–31. PubMed
- Young J. Moral panic: its origins in resistance, ressentiment and the translation of fantasy into reality. Br J Criminol. 2009;49(1):4–16.
- Barnett BS, Arakelian M, Beebe D, et al. American psychiatrists’ opinions about classic hallucinogens and their potential therapeutic applications: a 7-year follow up survey. Psychedelic Med. 2024;2(1):1–9.
- Goodwin GM, Aaronson ST, Alvarez O, et al. Single-dose psilocybin for a treatment-resistant episode of major depression. N Engl J Med. 2022;387(18):1637–1648. PubMed CrossRef
- Raison CL, Sanacora G, Woolley J, et al. Single-dose psilocybin treatment for major depressive disorder: a randomized clinical trial. JAMA. 2023;330(9):843–853. PubMed CrossRef
- Bogenschutz MP, Ross S, Bhatt S, et al. Percentage of heavy drinking days following psilocybin-assisted psychotherapy vs placebo in the treatment of adult patients with alcohol use disorder: a randomized clinical trial. JAMA Psychiatry. 2022;79(10):953–962. PubMed CrossRef
- Holze F, Gasser P, Müller F, et al. Lysergic acid diethylamide-assisted therapy in patients with anxiety with and without a life-threatening illness: a randomized, double-blind, placebo-controlled phase II study. Biol Psychiatry. 2023;93(3):215–223. PubMed CrossRef
- Mitchell JM, Bogenschutz M, Lilienstein A, et al. MDMA-assisted therapy for severe PTSD: a randomized, double-blind, placebo-controlled phase 3 study. Nat Med. 2021;27(6):1025–1033. PubMed CrossRef
- Mitchell JM, Marcela Ot’alora M, van der Kolk B, et al. MDMA-assisted therapy for moderate to severe PTSD: a randomized, placebo-controlled phase 3 trial. Nat Med. 2023;29(10):2473–2480. PubMed CrossRef
- Danforth AL, Struble CM, Yazar-Klosinski B, et al. MDMA-assisted therapy: a new treatment model for social anxiety in autistic adults. Prog Neuropsychopharmacol Biol Psychiatry. 2016;64:237–249. PubMed CrossRef
- Sessa B, Higbed L, O’Brien S, et al. First study of safety and tolerability of 3,4-methylenedioxymethamphetamine-assisted psychotherapy in patients with alcohol use disorder. J Psychopharmacol. 2021;35(4):375–383. PubMed CrossRef
- Monson CM, Wagner AC, Mithoefer AT, et al. MDMA-facilitated cognitive behavioural conjoint therapy for posttraumatic stress disorder: an uncontrolled trial. Eur J Psychotraumatol. 2020;11(1):1840123. PubMed CrossRef
- Moreno FA, Wiegand CB, Taitano EK, et al. Safety, tolerability, and efficacy of psilocybin in 9 patients with obsessive-compulsive disorder. J Clin Psychiatry. 2006;67(11):1735–1740. PubMed CrossRef
- ClinicalTrials.gov. Psilocybin-facilitated treatment for chronic pain. Accessed May 24, 2024. https://www.clinicaltrials.gov/study/NCT05068791?term=psilocybin%20functional%20neurologic&rank=8
- ClinicalTrials.gov. Assessment of psilocybin (TRP-8802) in concert with psychotherapy in patients with irritable bowel syndrome (IBS). Accessed May 24, 2024. https://www.clinicaltrials.gov/study/NCT06206265?term=NCT06206265&rank=1
- Floriano I, Silvinato A, Bernardo WM. The use of esketamine in the treatment of patients with severe depression and suicidal ideation: systematic review and meta-analysis. Rev Assoc Med Bras (1992). 2023;69(4):e2023D694. PubMed CrossRef
- Marcantoni WS, Akoumba BS, Wassef M, et al. A systematic review and meta analysis of the efficacy of intravenous ketamine infusion for treatment resistant depression: January 2009 - January 2019. J Affect Disord. 2020;277:831–841. PubMed CrossRef
- Witt K, Potts J, Hubers A, et al. Ketamine for suicidal ideation in adults with psychiatric disorders: a systematic review and meta-analysis of treatment trials. Aust N Z J Psychiatry. 2020;54(1):29–45. PubMed CrossRef
- Holze F, Ley L, Müller F, et al. Direct comparison of the acute effects of lysergic acid diethylamide and psilocybin in a double-blind placebo-controlled study in healthy subjects. Neuropsychopharmacology. 2022;47(6):1180–1187. PubMed CrossRef
- Holze F, Vizeli P, Muller F, et al. Distinct acute effects of LSD, MDMA, and d amphetamine in healthy subjects. Neuropsychopharmacology. 2020;45(3):462–471. PubMed CrossRef
- Suleiman Z, Ik K, Bo B. Evaluation of the cardiovascular stimulation effects after induction of anaesthesia with ketamine. J West Afr Coll Surg. 2012;2(1):38–52. PubMed
- Riva-Posse P, Reiff CM, Edwards JA, et al. Blood pressure safety of subanesthetic ketamine for depression: a report on 684 infusions. J Affect Disord. 2018;236:291–297. PubMed CrossRef
- Chang M, Juruena MF, Young AH. Ketamine cystitis following ketamine therapy for treatment-resistant depression - case report. BMC Psychiatry. 2024;24(1):9. PubMed
- Mueller PD, Korey WS. Death by “ecstasy”: the serotonin syndrome? Ann Emerg Med. 1998;32(3):377–380. PubMed
- Budisavljevic MN, Stewart L, Sahn SA, et al. Hyponatremia associated with 3,4- methylenedioxymethylamphetamine (“ecstasy”) abuse. Am J Med Sci. 2003;326(2):89–93. PubMed
- Simonsson O, Goldberg SB, Chambers R, et al. Prevalence and associations of classic psychedelic-related seizures in a population-based sample. Drug Alcohol Depend. 2022;239:109586. PubMed CrossRef
- Koenig X, Hilber K. The anti-addiction drug ibogaine and the heart: a delicate relation. Molecules. 2015;20(2):2208–2228. PubMed CrossRef
- Alper KR, Stajić M, Gill JR. Fatalities temporally associated with the ingestion of ibogaine. J Forensic Sci. 2012;57(2):398–412. PubMed CrossRef
- Cherian KN, Keynan JN, Anker L, et al. Magnesium-ibogaine therapy in veterans with traumatic brain injuries. Nat Med. 2024;30(2):373–381. PubMed CrossRef
- Ling S, Ceban F, Lui LMW, et al. Molecular mechanisms of psilocybin and implications for the treatment of depression. CNS Drugs. 2022;36(1):17–30. PubMed
- Cao C, Barros-Álvarez X, Zhang S, et al. Signaling snapshots of a serotonin receptor activated by the prototypical psychedelic LSD. Neuron. 2022;110(19):3154–3167.e7. PubMed CrossRef
- Luethi D, Kolaczynska KE, Walter M, et al. Metabolites of the ring-substituted stimulants MDMA, methylone and MDPV differentially affect human monoaminergic systems. J Psychopharmacol. 2019;33(7):831–841. PubMed CrossRef
- Connolly HM, Crary JL, McGoon MD, et al. Valvular heart disease associated with fenfluramine-phentermine. N Engl J Med. 1997;337(9):581–588. PubMed CrossRef
- Libânio Osório Marta RF. Metabolism of lysergic acid diethylamide (LSD): an update. Drug Metab Rev. 2019;51(3):378–387. PubMed
- Dinis-Oliveira RJ. Metabolism of psilocybin and psilocin: clinical and forensic toxicological relevance. Drug Metab Rev. 2017;49(1):84–91. PubMed CrossRef
- Dishotsky NI, Loughman WD, Mogar RE, et al. LSD and genetic damage. Science. 1971;172(3982):431–440. PubMed CrossRef
- Barnett BS, Ziegler K, Doblin R, et al. Is psychedelic use associated with cancer?: interrogating a half-century-old claim using contemporary population-level data. J Psychopharmacol. 2022;36(10):1118–1128. PubMed CrossRef
- Ricaurte GA, Yuan J, Hatzidimitriou G, et al. Retracted: severe dopaminergic neurotoxicity in primates after a common recreational dose regimen of MDMA (“ecstasy”). Science. 2002;297(5590):2260–2263. PubMed CrossRef
- Barnett BS, Doblin R. Dissemination of erroneous research findings and subsequent retraction in high-circulation newspapers: a case study of alleged MDMA-induced dopaminergic neurotoxicity in primates. J Psychoactive Drugs. 2021;53(2):104–110. PubMed CrossRef
- Carbonaro TM, Bradstreet MP, Barrett FS, et al. Survey study of challenging experiences after ingesting psilocybin mushrooms: acute and enduring positive and negative consequences. J Psychopharmacol. 2016;30(12):1268–1278. PubMed CrossRef
- Gorman I, Nielson EM, Molinar A, et al. Psychedelic harm reduction and integration: a transtheoretical model for clinical practice. Front Psychol. 2021;12:645246. PubMed CrossRef
- Kramer EN, Reddy K, Shapiro B. A suicide attempt following psilocybin ingestion in a patient with no prior psychiatric history. Psychiatry Res Case Rep. 2023;2(1):100118.
- Frosch WA, Robbins ES, Stern M. Untoward reactions to lysergic aciddiethylamide (LSD) resulting in hospitalization. N Engl J Med. 1965;273(23):1235–1239. PubMed CrossRef
- Nutt DJ, King LA, Phillips LD, et al. Drug harms in the UK: a multicriteria decision analysis. Lancet. 2010;376(9752):1558–1565. PubMed CrossRef
- Schifano F. Potential human neurotoxicity of MDMA (“ecstasy”): subjective self reports, evidence from an Italian drug addiction centre and clinical case studies. Neuropsychobiology. 2000;42(1):25–33. PubMed CrossRef
- Liu Y, Lin D, Wu B, et al. Ketamine abuse potential and use disorder. Brain Res Bull. 2016;126(Pt 1):68–73. PubMed CrossRef
- Simonsson O, Mosing MA, Osika W, et al. Adolescent psychedelic use and psychotic or manic symptoms. JAMA Psychiatry. 2024;81:579–585. PubMed CrossRef
- Honk L, Stenfors CUD, Goldberg SB, et al. Longitudinal associations between psychedelic use and psychotic symptoms in the United States and the United Kingdom. J Affect Disord. 2024;351:194–201. PubMed
- Aaronson ST, van der Vaart A, Miller T, et al. Single-dose synthetic psilocybin with psychotherapy for treatment-resistant bipolar type ii major depressive episodes: a nonrandomized open-label trial. JAMA Psychiatry. 2024;81(6):555–562. PubMed
- Gukasyan N, Griffiths RR, Yaden DB, et al. Attenuation of psilocybin mushroom effects during and after SSRI/SNRI antidepressant use. J Psychopharmacol. 2023;37(7):707–716. PubMed CrossRef
- Becker AM, Holze F, Grandinetti T, et al. Acute effects of psilocybin after escitalopram or placebo pretreatment in a randomized, double-blind, placebo controlled, crossover study in healthy subjects. Clin Pharmacol Ther. 2022;111(4):886–895. PubMed CrossRef
- Goodwin GM, Croal M, Feifel D, et al. Psilocybin for treatment resistant depression in patients taking a concomitant SSRI medication. Neuropsychopharmacology. 2023;48(10):1492–1499. PubMed CrossRef
- Liechti ME, Vollenweider FX. The serotonin uptake inhibitor citalopram reduces acute cardiovascular and vegetative effects of 3,4- methylenedioxymethamphetamine (“ecstasy”) in healthy volunteers. J Psychopharmacol. 2000;14(3):269–274. PubMed CrossRef
- Pilgrim JL, Gerostamoulos D, Woodford N, et al. Serotonin toxicity involving MDMA (ecstasy) and moclobemide. Forensic Sci Int. 2012;215(1–3):184–188. PubMed CrossRef
- Nayak SM, Gukasyan N, Barrett FS, et al. Classic psychedelic coadministration with lithium, but not lamotrigine, is associated with seizures: an analysis of online psychedelic experience reports. Pharmacopsychiatry. 2021;54(5):240–245. PubMed CrossRef
- Vollenweider FX, Vollenweider-Scherpenhuyzen MF, Bäbler A, et al. Psilocybin induces schizophrenia-like psychosis in humans via a serotonin-2 agonist action. Neuroreport. 1998;9(17):3897–3902. PubMed CrossRef
- APA. Resource document on ethical and practical implications of psychedelics in psychiatry. American Psychiatric Association. Accessed May 24, 2024. https://www.psychiatry.org/getattachment/998071b6-138e-40d1-a482-e7b8e85d4f90/Resource-Document-Psychedelics-in-Psychiatry.pdf
- MAPS. Maps psychedelic integration station. Accessed July 29, 2024. https://maps.org/integration-station/
- JHMI. Psychedelic risks, side effects, and potential harms. Accessed May 24, 2024. https://www.youtube.com/watch?v=xUS2I8PNOH0
Enjoy this premium PDF as part of your membership benefits!