Lessons Learned at the Interface of Medicine and Psychiatry
The Psychiatric Consultation Service at Massachusetts General Hospital sees medical and surgical inpatients with comorbid psychiatric symptoms and conditions. During their twice-weekly rounds, Dr Stern and other members of the Consultation Service discuss diagnosis and management of hospitalized patients with complex medical or surgical problems who also demonstrate psychiatric symptoms or conditions. These discussions have given rise to rounds reports that will prove useful for clinicians practicing at the interface of medicine and psychiatry.
Prim Care Companion CNS Disord 2024;26(4):23f03692
Author affiliations are listed at the end of this article.
Have you been unclear about how treatment resistant schizophrenia (TRS) is defined? Have you been uncertain about how to evaluate a patient with a chronic psychotic illness? Have you struggled over which treatments you should consider when treating someone with TRS? If you have, the following case vignette and discussion should prove useful.
CASE VIGNETTE
Ms C, a 35-year-old woman, first became psychotic with auditory hallucinations and paranoia (ie, her neighbors were constantly communicating with her and trying to break into her house) during her sophomore year of college; she had also been using cannabis frequently. Despite stopping cannabis for more than 3 months, her psychosis persisted. She was initially treated with lurasidone (as she preferred a weight-neutral agent), but even with doses over 90 mg/d for 6 weeks, there was no improvement in her psychotic symptoms. She was switched to risperidone, and the dose was titrated to 3 mg at bedtime. Her hallucinations and paranoia subsided but failed to remit. When she felt somewhat better, she stopped her medications for several months; this led to a relapse and a lengthy hospitalization. Given her medication nonadherence as an inpatient, she was trialed on oral Invega and transitioned to a monthly long acting injectable (Invega Sustenna 234 mg) to ensure adherence. Even after getting monthly injections without interruption for 3 months, her symptoms persisted. Her outpatient psychiatrist started olanzapine (and titrated it to 20 mg/d) and discontinued the injections. Even with consistent adherence to olanzapine (20 mg/d) for 2 months, her symptoms showed only minimal responsiveness.
Ms C was diagnosed with TRS for having failed 2 nonclozapine antipsychotic trials (with adequate dose, duration, and adherence). She was encouraged to start clozapine, but due to the burden of regular blood work monitoring and her fear of weight gain, she did not agree to a clozapine trial for 6 months. Her executive function deteriorated, which resulted in her losing her job. Paranoia led her to call 9-1-1 multiple times each day to report her neighbors’ suspicious behaviors. She trespassed on her neighbor’s property and received a restraining order. Ultimately, she was hospitalized involuntarily.
DISCUSSION
What Is TRS?
Schizophrenia is a chronic, progressive psychiatric disorder characterized by symptoms that include hallucinations, delusions, disorganization, impaired motivation, deficits in self-expression, and cognitive impairment.1 Unfortunately, a subset of patients with schizophrenia do not respond to first-line treatments, which necessitates more complex clinical decision-making to limit morbidity and mortality.
In 2017, the Treatment Response and Resistance in Psychosis (TRRIP) Working Group published criteria for treatment resistance based on an international expert consensus.2 This group defined TRS by having at least moderate symptom severity and functional impairment due to schizophrenia, with an inadequate response to 2 or more antipsychotic medication trials. Validated scales should be used to measure and confirm symptom severity (eg, the Brief Psychiatric Rating Scale [BPRS])3 and functional impairment (eg, the Social and Occupational Functioning Assessment Scale).4 Each antipsychotic trial requires a sufficient dose (equivalent to at least 600 mg of chlorpromazine daily), duration (a minimum of 6 weeks), and patient adherence (at least 80% of prescribed doses taken). Of note, the above criteria represent minimal TRRIP benchmarks for diagnosing TRS; optimal TRRIP criteria also include prospective monitoring of symptom severity via a scale that confirms less than 20% symptom decrease over the antipsychotic course and confirmation of antipsychotic adherence via 2 or more plasma levels and trialing at least 1 long-acting injectable.
About one-third of patients with schizophrenia meet criteria for TRS, a high proportion of whom are treatment resistant from the onset of their psychotic illness (ie, primary TRS).5 Given that the duration of untreated psychosis and repeated psychotic episodes increases treatment resistance, identification of TRS and early intervention are necessary to improve treatment outcomes.6
What Looks Like TRS But Is Not?
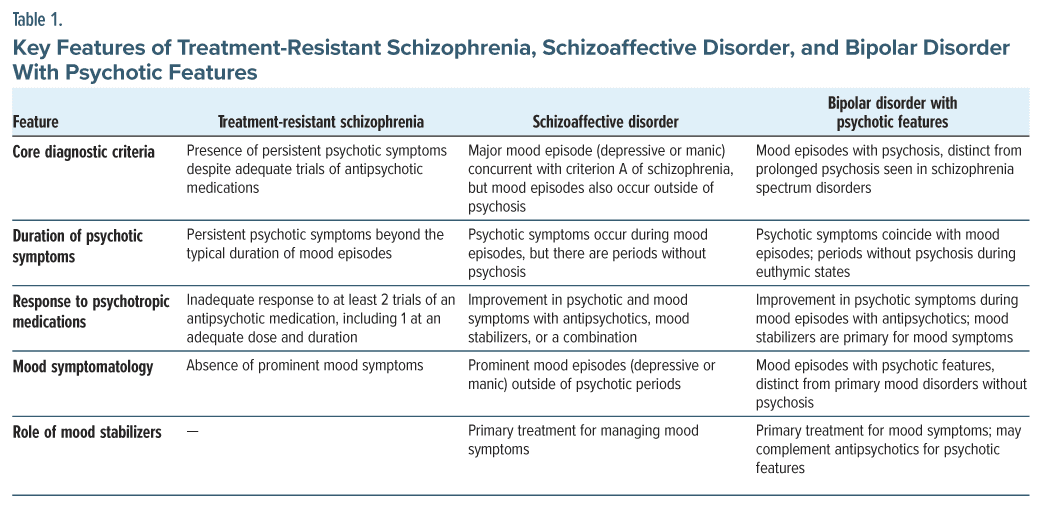
The differential diagnosis of TRS involves considering other key psychiatric conditions, such as schizoaffective disorder or bipolar disorder with psychotic features. Distinguishing between TRS and other psychiatric conditions can be challenging, as they share psychotic symptoms. Table 1 outlines the key features of TRS, schizoaffective disorder, and bipolar disorder with psychotic features.
What Does the Evaluation of TRS Involve?
The evaluation of TRS begins with a thorough review of the patient’s psychiatric and treatment history. All nonpsychiatric causes of psychosis should be ruled out before concluding that a person has TRS. Moreover, the patient should meet the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, criteria for schizophrenia.7 In addition, consensus criteria suggest that evidence-based, validated symptom rating scales, such as the Positive and Negative Syndrome Scale (PANSS),8 the BPRS,3 the Scale for the Assessment of Negative Symptoms (SANS),9 or the Scale for the Assessment of Positive Symptoms (SAPS),10 should be used to quantify current overall, positive, and negative symptom severity. Current symptom severity should be moderate (or higher) in at least 2 areas (eg, auditory hallucinations, delusions, and negative symptoms) or severe in 1 area.2
The evaluator must also determine that the patient has failed 2 or more antipsychotic trials that were adequate regarding the dose, duration, and adherence.2 To consider an antipsychotic trial as having failed, a patient’s symptoms should have improved by less than 20% or they must have continued to experience moderate symptoms in 2 or more areas or have severe symptoms in 1 area2 while taking an antipsychotic with adequate dose, duration, and adherence. An adequate duration is typically considered to be at least 6 weeks on a therapeutic dose (ie, at least 600-mg equivalents of chlorpromazine/day).2 Adequate adherence is defined as at least 80% of prescribed doses taken, as confirmed by at least 2 sources, including pill counts, dispensing chart review, or patient or caregiver report.2 In addition, antipsychotic drug levels should be monitored at least once during the medication trial.2 Multiple sources of information (including from the patient and their family and from medical records) may be used to determine the efficacy of a prior response. In addition, other factors (including active substance use or untreated medical problems) that may contribute to ongoing psychotic symptoms must also be ruled out.
What Kinds of Biological, Psychological, and Social Interventions Can Help to Manage TRS?
Patients with TRS should be offered a clozapine trial. It is the only US Food and Drug Administration (FDA)–approved antipsychotic medication for TRS, and it has superior efficacy when compared to all other antipsychotics.11 For patients with TRS, there is limited benefit obtained with use of other nonclozapine antipsychotics.12 The initial serum level target for clozapine is a trough level >250 ng/mL.2 If there is an insufficient response at this level, the dose should be increased to achieve a level >350 ng/mL.2 Monitoring of serum levels is crucial since individual factors (such as sex and cigarette smoking) can affect serum levels and therefore treatment response.2 A clozapine trial that lasts at least 3 months is required once therapeutic levels have been achieved.2
Some patients fail to respond adequately to clozapine. On the population level, augmentation with a second antipsychotic or another adjunctive medication is unlikely to be helpful, and there is no clear support for any augmentation strategy over another.13,14
Use of nonpharmacologic treatments should also be considered as adjunctive treatments. Electroconvulsive therapy (ECT) may be beneficial for people with TRS who have not achieved an adequate treatment response with clozapine. Up to 50% of patients with TRS improve with ECT.15 In addition, cognitive-behavioral therapy for psychosis has demonstrated moderate efficacy for patients with TRS.16 Transcranial magnetic stimulation (TMS) may offer some improvement in symptoms for people with medication-resistant auditory verbal hallucinations,17 although much of the literature has demonstrated mixed results regarding positive symptoms.18 Similarly, the literature regarding the effect of TMS on negative symptoms is also mixed.18,19 Finally, research has not demonstrated benefits associated with rehabilitative treatment in improving social functioning, such as increasing patients’ participation in activities in TRS.20
When Should Other Medications, Neuromodulatory Techniques, or Surgical Approaches Be Considered When Someone Is Thought to Have TRS?
An adequate trial of clozapine should be established before trying augmentation strategies. A clozapine trial should last at least 3–4 months with at least an 80% adherence rate and with a serum clozapine level >350 ng/mL.21 The clozapine dose should be increased to at least 450 ng/mL for nonresponders; however, neither upper levels for therapeutic benefits nor toxicity have been established, and the dose can be raised, as tolerated, if ongoing benefit is noted. Therapeutic drug monitoring is critical to confirm an adequate dosage and adherence because some patients may be rapid metabolizers of clozapine, drug-drug interactions may arise, and tobacco use can decrease clozapine levels.22 Nevertheless, about half of those with TRS have clozapine-resistant schizophrenia (ie, they show minimal or no symptomatic response to clozapine and require adjunctive treatments).
After optimizing the clozapine dosage, several strategies can be considered for persistent symptoms. ECT is the evidence-based treatment for clozapine resistant schizophrenia. Symptom improvement of 40%–50% has been noted with ECT.15 However, ECT is not always immediately available, and patients often do not agree with its use; in the interim, pharmacologic augmentation strategies are often tried for patients who continue to take clozapine. Although there were promising trials of clozapine augmentation with less invasive repetitive TMS, a meta-analysis found no evidence of effectiveness for psychotic symptoms.21 In terms of medications, adjunctive aripiprazole can reduce psychotic symptoms, mitigate metabolic side effects of clozapine, improve mood and negative symptoms, and serve as an augmentation strategy to lower the risk of psychiatric rehospitalization compared to clozapine monotherapy.23 The data regarding the effectiveness of mood stabilizers as augmentation therapy are mixed and contradictory. Among the most widely studied mood stabilizers for augmenting clozapine are lamotrigine, topiramate, lithium, and valproic acid; however, further research is needed to reach definitive conclusions. Valproic acid appears to have a calming effect on patients experiencing acute psychosis accompanied by hostility, but its long-term effect is less clear.24
How Can Family Members of Those With TRS Become Better Prepared to Help Their Loved Ones?
Navigating the complexities of coping with TRS poses significant challenges for both affected individuals and their familial support networks. To better prepare their loved ones who are struggling with TRS, family members should acquire knowledge about TRS. Accompanying affected individuals during a routine health care appointment allows family members to gain critical insights into the fundamental aspects of TRS, its symptomatic manifestations, and the spectrum of available treatment modalities. Research also suggests that most families of patients with TRS report that they have received inadequate information regarding the early warning signs of relapse, side effects of medications, and ways that they can cope with violent behaviors.25 To address these issues, during interactions with health care professionals, family members should discuss how to recognize early signs of psychotic decompensation, which can lead to timely intervention and support. In addition, families should be equipped with de-escalation strategies to handle potential crises effectively, particularly when patients struggle with paranoia or engage in fear-related physical protective responses. There are often local chapters of nationwide organizations, such as the National Alliance on Mental Illness (NAMI), that can help patients and their families (ie, Family to Family programs help family members best support patients). It is imperative for families to identify nonpolice emergency response resources within their community to ensure appropriate assistance during crises, minimizing the risk of misinterpretation and escalation in potentially volatile situations. This collaborative approach empowers family members to initiate timely interventions, thereby mitigating the impact of crises and improving the overall quality of life for their loved ones.
In addition, effective communication plays a crucial role in supporting individuals who are grappling with TRS. It would be advantageous for family members to enhance their communication skills; this may help to establish a secure environment that encourages open and honest conversation between loved ones and their family members and allows affected individuals to express their thoughts and emotions without restriction.
While assisting loved ones who are struggling with TRS, family members should prioritize their own mental health and well-being. For example, research suggests that persistent positive symptoms and frequent relapses associated with TRS has been linked to a perceived burden, which results in feeling overwhelmed with a lack of relief and takes a toll on the emotional and physical health of caregivers.26 Participating in support groups or seeking guidance from mental health professionals enables family members to develop invaluable coping strategies. This approach serves not only to prevent the worsening of mental and emotional health but also to help sustain resilience among family members, which is required for supporting a loved one with TRS over an extended period.
Case Vignette: What Happened to Ms C?
Eventually, Ms C agreed to a clozapine trial. Therapeutic drug monitoring of clozapine blood levels was used to avoid both toxic and subtherapeutic levels, and the dose was titrated to a target of 350 ng/mL (with a clozapine dose of 400 mg/d). However, she continued to struggle with paranoia. She benefited from raising the clozapine dose to 500 mg/d, which led to a serum clozapine level of 450 ng/mL. However, this dose/level made her too sedated and constipated, and she was drooling excessively; these symptoms were managed with laxatives and glycopyrrolate, respectively. However, severe fatigue prevented her from returning to work, and her clozapine dose was reduced to 400 mg/d and aripiprazole was added, which improved her psychotic symptoms, energy level, and mood and also mitigated further weight gain.
CONCLUSION
Schizophrenia is a chronic, progressive psychiatric disorder characterized by hallucinations, delusions, disorganization, impaired motivation, deficits in self expression, and cognitive impairment. TRS is defined by having at least moderate symptom severity and functional impairment due to schizophrenia, with an inadequate response to 2 or more antipsychotic medication trials. Assessment and monitoring should be accomplished with the aid of validated symptom rating scales (such as the PANSS, the BPRS, the SANS, or the SAPS) to quantify current overall, positive, and negative symptom severity. When individuals have TRS, they should be offered a clozapine trial; it is the only FDA-approved antipsychotic medication for TRS, and it has superior efficacy when compared to all other antipsychotics. In addition, cognitive-behavioral therapy for psychosis has demonstrated moderate efficacy for patients with TRS. Moreover, effective communication plays a crucial role in supporting individuals who are grappling with TRS.
Article Information
Published Online: July 2, 2024. https://doi.org/10.4088/PCC.23f03692
© 2024 Physicians Postgraduate Press, Inc.
Submitted: December 26, 2023; accepted March 12, 2024.
To Cite: Lim CS, Donovan AL, Vyas CM, et al. Treatment-resistant schizophrenia: evaluation and management. Prim Care Companion CNS Disord. 2024;26(4):23f03692.
Author Affiliations: Department of Psychiatry, Massachusetts General Hospital, Boston, Massachusetts (all authors); Harvard Medical School, Boston, Massachusetts (all authors).
Corresponding Author: Carol S. Lim, MD, MPH, Department of Psychiatry, Massachusetts General Hospital, 151 Merrimac St, 4th Floor, Boston, MA 02114 ([email protected]).
Drs Lim, Donovan, Vyas, Daneshvari, and Lissanu are co-first authors.
Relevant Financial Disclosures: Dr Lim reports receiving research grants from Karuna, Merck, and Neurocrine; consultant honoraria from Karuna; and medical honoraria from MDedge and Hatherleigh. Dr Vyas has received research support from Nestlé-Purina Petcare Company, Mars Edge, and American Foundation for Suicide Prevention. The other authors report no conflicts with any product mentioned or concept discussed in this article and have no disclosures.
Funding/Support: None.
Clinical Points
- Treatment-resistant schizophrenia is defined by having at least moderate symptom severity and functional impairment due to schizophrenia, with an inadequate
response to 2 or more antipsychotic medication trials. - Validated scales should be used to measure and confirm symptom severity.
- Each antipsychotic trial requires a dose that is equivalent to ≥600 mg/d of chlorpromazine, for a minimum of 6 weeks, and with at least 80% of prescribed doses taken.
- Therapeutic drug monitoring is critical to confirm an adequate dosage and adherence because some patients may be rapid metabolizers of clozapine, drug-drug interactions may arise, and tobacco use can decrease clozapine levels.
- After optimizing the clozapine dosage, several interventions (eg, use of electroconvulsive therapy, augmentation with mood stabilizers, participation in support groups, and obtaining guidance from mental health professionals) can facilitate improvement in patients and their family members.
References (26)

- McCutcheon RA, Reis Marques T, Howes OD. Schizophrenia-an overview. JAMA Psychiatry. 2020;77(2):201–210. PubMed
- Howes OD, McCutcheon R, Agid O, et al. Treatment-resistant schizophrenia: Treatment Response and Resistance In Psychosis (TRRIP) working group consensus guidelines on diagnosis and terminology. Am J Psychiatry. 2017;174(3):216–229. PubMed CrossRef
- Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. PsycholRep. 1962;10(3):799–812.
- Morosini PL, Magliano L, Brambilla L, et al. Development, reliability, and acceptability of a new version of the DSM-IV Social and Occupational Functioning Assessment Scale (SOFAS) to assess routine social functioning. Acta Psychiatr Scand. 2000;101(4):323–329. PubMed
- Demjaha A, Lappin JM, Stahl D, et al. Antipsychotic treatment resistance in first episode psychosis: prevalence, subtypes and predictors. Psychol Med. 2017;47(11):1981–1989. PubMed CrossRef
- Howes OD, Whitehurst T, Shatalina E, et al. The clinical significance of duration of untreated psychosis: an umbrella review and random-effects meta-analysis. World Psychiatry. 2021;20(1):75–95. PubMed
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th rev ed; 2022. https://doi.org/10.1176/appi.books.9780890425787
- Kay SR, Fiszbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276. PubMed
- Andreasen NC. Scale for the Assessment of Negative Symptoms. University of Iowa; 1984.
- Andreasen NC. Scale for the Assessment of Positive Symptoms. University of Iowa; 1984.
- Huhn M, Nikolakopoulou A, Schneider-Thoma J, et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi episode schizophrenia: a systematic review and network meta-analysis. Lancet. 2019;394(10202):939–951. PubMed CrossRef
- Kane JM, Agid O, Baldwin ML, et al. Clinical guidance on the identification and management of treatment-resistant schizophrenia. J Clin Psychiatry. 2019;80(2): 18com12123. PubMed
- Correll CU, Rubio JM, Inczedy-Farkas G, et al. Efficacy of 42 Pharmacologic cotreatment strategies added to antipsychotic monotherapy in schizophrenia: systematic overview and quality appraisal of the meta-analytic evidence. JAMA Psychiatry. 2017;74(7):675–684. PubMed CrossRef
- Galling B, Roldán A, Hagi K, et al. Antipsychotic augmentation vs. monotherapy in schizophrenia: systematic review, meta-analysis and meta-regression analysis. World Psychiatry. 2017;16(1):77–89. PubMed CrossRef
- Petrides G, Malur C, Braga RJ, et al. Electroconvulsive therapy augmentation in clozapine-resistant schizophrenia: a prospective, randomized study. Am J Psychiatry. 2015;172(1):52–58. PubMed CrossRef
- Burns AMN, Erickson DH, Brenner CA. Cognitive-behavioral therapy for medication-resistant psychosis: a meta-analytic review. Psychiatr Serv. 2014;65(7):874–880. PubMed CrossRef
- Slotema CW, Blom JD, van Lutterveld R, et al. Review of the efficacy of transcranial magnetic stimulation for auditory verbal hallucinations. Biol Psychiatry. 2014;76(2):101–110. PubMed CrossRef
- Mehta UM, Naik SS, Thanki MV, et al. Investigational and therapeutic applications of transcranial magnetic stimulation in schizophrenia. Curr Psychiatry Rep. 2019;21(9):89. PubMed
- Patel S, Silvi S, Desai S, et al. Effectiveness of repetitive transcranial magnetic stimulation in depression, schizophrenia, and obsessive-compulsive disorder: an umbrella meta-analysis. Prim Care Companion CNS Disord. 2023;25(5):22r03423. PubMed
- Killaspy H, Marston L, Green N, et al. Clinical effectiveness of a staff training intervention in mental health inpatient rehabilitation units designed to increase patients’ engagement in activities (the Rehabilitation Effectiveness for Activities for Life [REAL] study): single-blind, cluster-randomised controlled trial. Lancet Psychiatry. 2015;2(1):38–48. PubMed CrossRef
- Chakrabarti S. Clozapine resistant schizophrenia: newer avenues of management. World J Psychiatry. 2021;11(8):429–448. PubMed
- Freudenreich O, Schnitzer K. How to use clozapine: a primer for clinicians [Hatherleigh CME Lessons]. Dir Psychiatry. 2021;41(1):15–30.
- Tiihonen J, Taipale H, Mehtälä J, et al. Association of antipsychotic polypharmacy vs monotherapy with psychiatric rehospitalization among adults with schizophrenia. JAMA Psychiatry. 2019;76(5):499–507. PubMed
- Porcelli S, Balzarro B, Serretti A. Clozapine resistance: augmentation strategies. Eur Neuropsychopharmacol. 2012;22(3):165–182. PubMed
- Lippi G. Schizophrenia in a member of the family: burden, expressed emotion and addressing the needs of the whole family. S Afr J Psychiatr. 2016;22(1):922. PubMed CrossRef
- Brain C, Kymes S, DiBenedetti DB, et al. Experiences, attitudes, and perceptions of caregivers of individuals with treatment-resistant schizophrenia: a qualitative study. BMC Psychiatry. 2018;18(1):253. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!