Abstract
Objective: To design and conduct a survey-based study to understand what internists and neurologists know and think about catatonia, with the goal of raising catatonia awareness among these practitioners and informing future educational campaigns.
Methods: The authors disseminated an online catatonia survey and educational module of the Bush-Francis Catatonia Rating Scale (BFCRS) via X/Twitter, professional listservs, and newsletters, from September 5, 2023, to January 15, 2024. Attendings, fellows, residents, and advanced-practice providers in internal medicine or neurology were eligible. Results on catatonia knowledge and attitudes are described and evaluated for associations with self-reported demographics. BFCRS scoring accuracy of this study’s cohort is compared with a prior cohort of psychiatric practitioners.
Results: Of the 64 eligible respondents, 58 completed the questionnaire, and 38 scored the test patient video. Most participants correctly identified medical sequelae of catatonia and benzodiazepines as the first-line treatment. However, whereas most agreed that practitioners in their specialty should know about catatonia and that it would be beneficial for them to receive catatonia training, only 16 (18%) completed the educational modules. Overall performance in this sample did not differ based on specialty, stage of training, or years of practice. The mean correct score on the BFCRS was 14 of 23, which was statistically lower than that of a historical psychiatry cohort (P < .001).
Conclusions: Although participants correctly identified medical sequelae and first-line treatment of catatonia, large gaps in catatonia-related knowledge were identified. The low participation rate and high attrition, despite widespread affirmation of catatonia’s importance to their specialty, may reflect attitudes about catatonia. These results call for education on catatonia recognition and greater awareness of catatonia among internists and neurologists.
Prim Care Companion CNS Disord 2025;27(2):24m03853
Author affiliations are listed at the end of this article.
Catatonia is a potentially life-threatening psychomotor syndrome that can arise from a variety of primary psychiatric conditions, medical and neurological conditions, or as an adverse effect of medications.1 Prompt identification of catatonia is essential to guide diagnostic workup, to ensure access to effective catatonia-specific treatments, and to inform clinical management, including prevention of its potential sequelae.2
Catatonia is often regarded as the exclusive purview of psychiatry; however, it can be the chief presenting clinical manifestation of many medical or neurological conditions unrelated to a primary psychiatric condition. Although hospital-wide estimates of catatonia prevalence are compromised by under-recognition, a study found features of catatonia in roughly one-third of intensive care unit patients.3 A review of pooled reports across all clinical settings found that 1 in 5 cases of catatonia has a secondary nonpsychiatric cause.4 In acute medical settings, half of reported catatonia cases are secondary to a medical cause, and, among critically ill and hospitalized older adults, secondary causes account for up to 80% of cases.5 Two-thirds of these secondary causes directly affect the brain and include encephalitis, neural injury, structural brain pathology, and seizures.5 As such, acute care practitioners in internal medicine and neurology are involved in the care of patients with catatonia and will often be the first clinicians to encounter patients with catatonia.
It is imperative that clinicians who encounter patients with catatonia be aware of its clinical features to ensure prompt recognition and treatment planning. There is a widespread gap in clinical practice regarding catatonia identification. Previous studies have reported that psychiatrists miss up to 90% of catatonia during routine care,6,7 and nonpsychiatric practitioners likely miss catatonia more frequently than psychiatrists.8 The Bush Francis Catatonia Rating Scale (BFCRS) is the most widely used standardized scale to assess for catatonia.9 We have shown that a brief online educational module on administering the BFCRS improves clinicians’—from medical students to attending psychiatrists—abilities to correctly identify features of catatonia.10 Education on the use of the BFCRS is a critical component in ensuring accurate catatonia identification and prompt treatment.
To our knowledge, there have been no prior studies evaluating both the knowledge of and attitudes toward catatonia among residents, fellows, attendings, and advanced-practice providers (APPs) in internal medicine and neurology. We designed and conducted a survey based study to understand what internists and neurologists know and think about catatonia. Our goals were to raise catatonia awareness among these practitioners and to inform future educational campaigns.
METHODS
We conducted an online study via REDCap, a secure web application used to build and manage online surveys. The study was divided into 2 phases: (1) prelearning module and (2) learning module. Training and assessment resources developed at the University of Rochester were utilized for this study (available at http://bfcrs.urmc.edu).10 We designed a questionnaire to assess practitioners’ experience with attitudes toward and knowledge of catatonia. Questionnaire iterations were piloted with medical students, residents in psychiatry, and faculty members at our institution. Our study was found to be exempt from formal review by the University of Rochester Medical Center Research Subject Review Board, as it did not qualify as human subject research (STUDY 8603).
To assess participants’ baseline proficiency with the BFCRS, we showed a video of a standardized test patient depicting key features of catatonia as elicited by the examiner. Participants were asked to score the test patient on each of the 23 items on the BFCRS using “Standardized Test Patient A” as previously studied.11
We disseminated a link to participate via X/Twitter, academic society newsletters, and message boards, enriched by snowballing (listed under Acknowledgments). Enrollment was open from September 5, 2023, to January 15, 2024. Prospective subjects were incentivized to participate. Those who completed the full study were entered into a raffle to receive one of three $100 Amazon gift cards.
Data from only self-identified attendings, fellows, residents, and APPs in neurology and internal medicine were included for analysis. Given attrition at each study stage, sample demographics are described at each of the 3 main prelearning module study time points: (1) demographics completion, (2) Catatonia Experience, Impressions, and Applications questionnaire completion, and (3) BFCRS Test Patient scoring completion.
We summed the 7 knowledge-based items in the Catatonia Experience, Impressions, and Applications questionnaire. One of these items contained 6 correct answer choices, so the maximum score possible was 13. We elicited attitudes toward catatonia via Likert scale items. All between-group comparisons were calculated using Fisher exact test because the data were not normally distributed. We evaluated whether participants’ catatonia knowledge scores and Likert scale responses were associated with self-reported demographics. We used χ2 tests to evaluate the likelihood of participants’ completing the educational module based on their responses regarding the importance of learning about catatonia.
Participants who scored the BFCRS Test Patient received 1 point for each correct item. We dichotomized scoring for each item based on its presence or absence in the video. For example, on the BFCRS, verbigeration can be scored as absent, occasional, frequent, or constant. However, for this study, if verbigeration was present in the video, individuals who selected any frequency other than absent received a point for the item.
Using independent samples t-tests, we compared BFCRS Test Patient scores from participants in this current study with the scores by psychiatric clinicians from a prior study (excluding medical students) that used the same test patient video (Standardized Test Patient A).11 Statistical significance was considered at P < .05. Analyses were completed using SPSS Statistics, version 29.0.0.0 (241) (IBM, Armonk, New York).
RESULTS
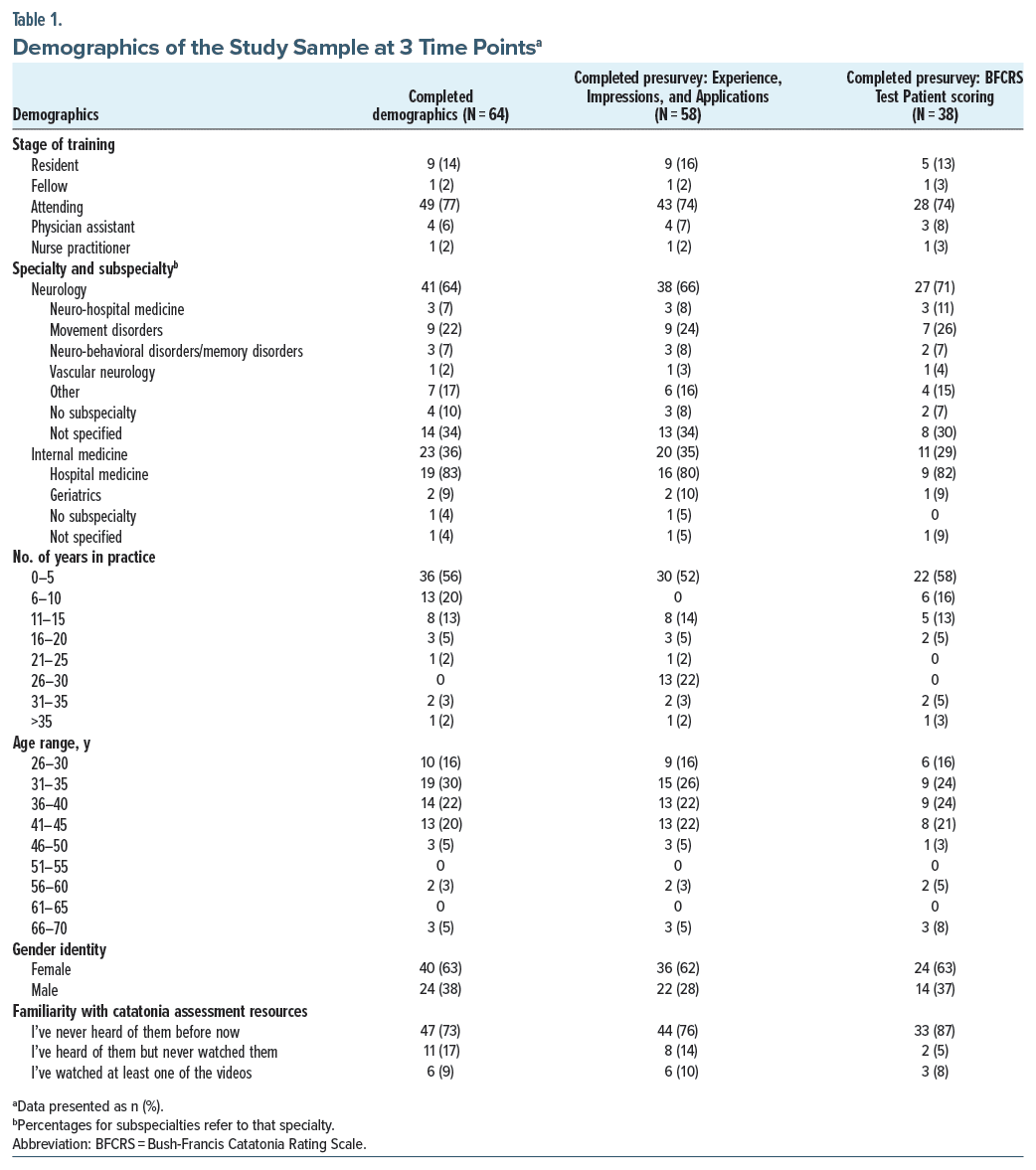
One hundred individuals opened the study information page; 99 consented to participate. Eleven participants were excluded from analysis for ineligibility. The number of participants who completed each stage of the study were as follows: study eligible (n = 88), completed demographics (n = 64, 73% of study eligible), completed Catatonia Experience, Impressions, and Applications questionnaire (n = 58, 66%), scored BFCRS Test Patient (n = 38, 43%), and completed learning module (n = 16, 18%). Study sample demographics at 3 main study time points are included in Table 1.
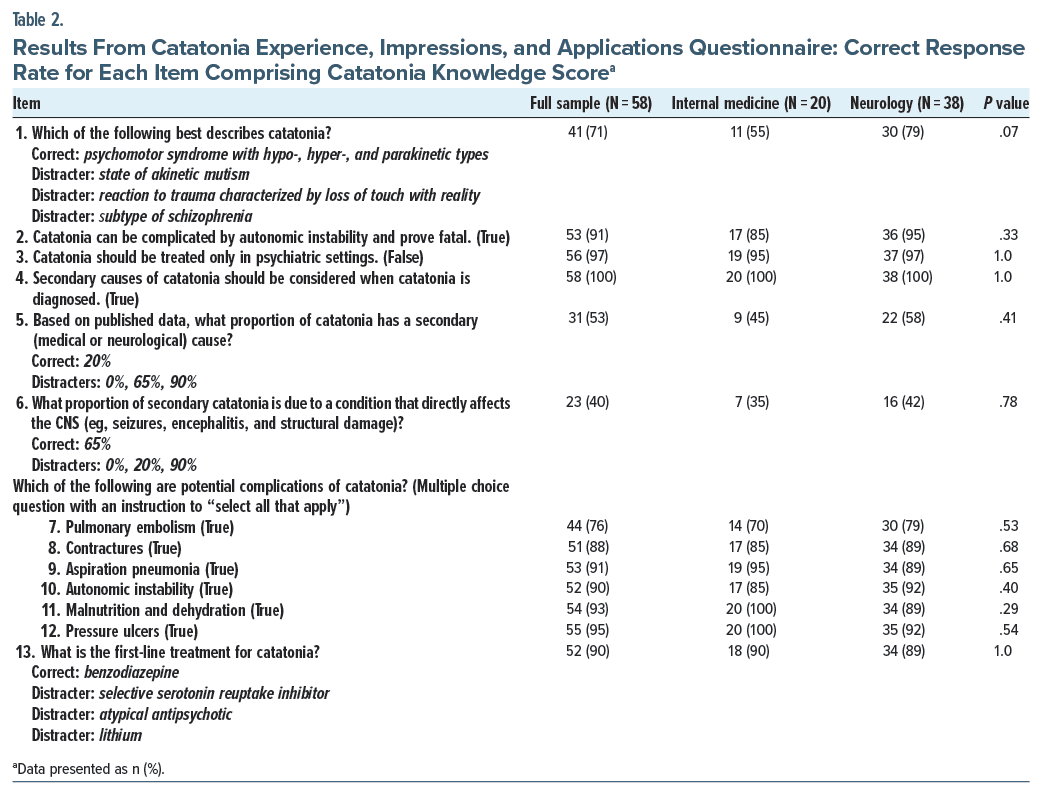
The mean catatonia knowledge score was 11 (SD = 2) out of a possible 13 points (82%). Overall performance on multiple-choice questions did not differ statistically based on specialty, stage of training, gender, age range, or years in practice (data not shown). The proportions of participants who answered each of the 13 individual items correctly, stratified by specialty, are shown in Table 2. No significant differences were found when comparing knowledge responses from neurology and internal medicine practitioners.
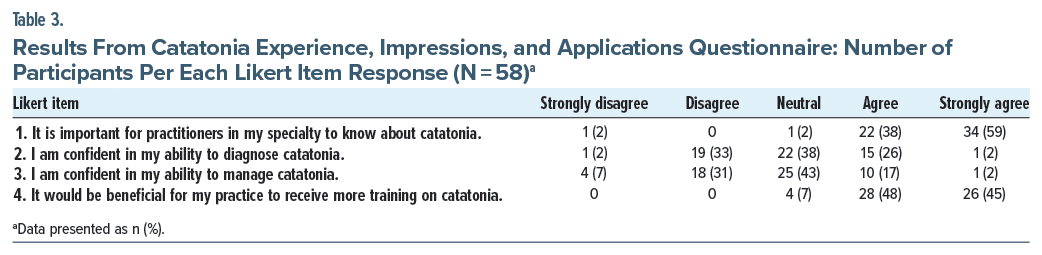
Responses to Likert scale questions for the full sample are shown in Table 3. Notably, 56 (97%) participants agreed with the statement “It is important for practitioners in my specialty to know about catatonia” (Likert 1), and 54 (93%) agreed with the statement “It would be beneficial for my practice to receive more training on catatonia” (Likert 4). Responses to Likert scale items did not differ based on participant stage of training or specialty (data not shown). Sixteen participants (25% of those who completed the demographics questionnaire) completed both learning modules. Participants’ likelihood of completing the BFCRS test subject scoring was not associated with their responses on Likert item 1 (P = .44) or Likert item 4 (P = .12).
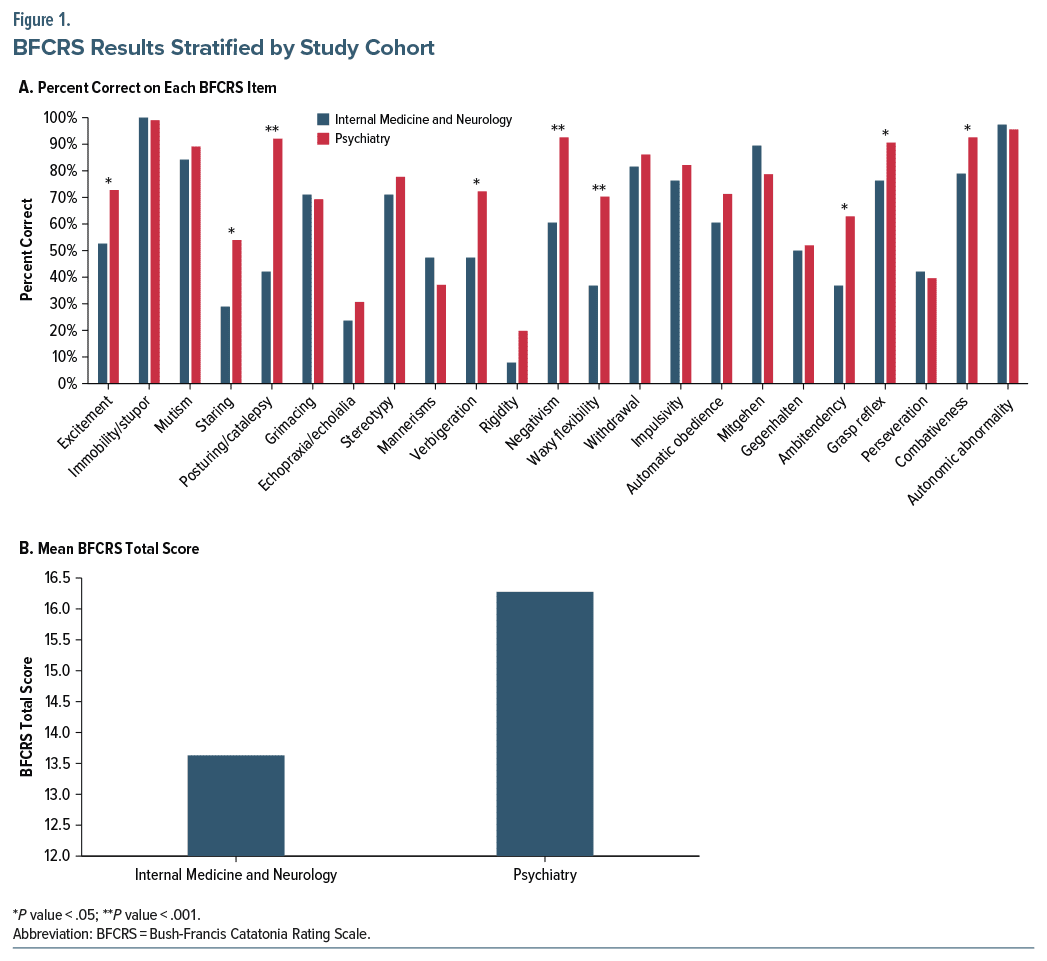
The full cohort mean correct score on the BFCRS Test Patient scoring module was 13.6 (SD = 2.6) out of 23 points (59%), which was similar regardless of specialty, stage of training, and gender (data not shown). The percentage of respondents who got each item of the BFCRS correct, stratified by specialty (internal medicine and neurology vs psychiatry), is shown in Figure 1A.11 Values from this figure are included in Supplementary Table 1. Of the 23 items on the BFCRS, 8 were correctly identified by less than half of current study participants. There was a significant difference in mean overall performance between the current cohort of internal medicine and neurology practitioners and a historical cohort of psychiatry practitioners (13.6 vs 16.3 correct, P < .001; Figure 1B).
DISCUSSION
Although it is reassuring that most internal medicine and neurology participants correctly identified the potential medical complications of catatonia, we identified several important gaps in catatonia-related knowledge. For instance, only half (53%) of participants correctly identified what proportion of catatonia has a secondary (medical or neurological) cause, and only 40% correctly identified what proportion of secondary catatonia is due to a condition that directly affects the central nervous system. Scores on knowledge-based items did not improve by stage of training (attending vs trainee) or differ by specialty (internal medicine vs neurology), gender (women vs men), age range, and years in practice.
Crucially, the first step in providing care for a patient with catatonia is identifying it, and the average internal medicine and neurology provider correctly identified only 59% (13.6/23) of items on the BFCRS Test Patient video, which did not differ by stage of training or years in practice. The most common, incorrectly scored catatonia findings based on the Test Patient video were rigidity (8% correct), echopraxia/echolalia (24%), and staring (29%). Our prior work revealed that the most common, incorrectly scored findings among psychiatric practitioners were rigidity (20% correct), echopraxia/echolalia (31%), and mannerisms (37%).11 Although we found gaps in catatonia knowledge among psychiatric practitioners as well, psychiatry practitioners scored significantly higher than the current study cohort on a broad range of BFCRS items including excitement, staring, posturing/catalepsy, verbigeration, negativism, waxy flexibility, ambitendency, grasp reflex, and combativeness.
Our findings are consistent with a prior study that evaluated catatonia knowledge among psychiatry and internal medicine residents and found that psychiatry residents scored better than internal medicine residents.12 To our knowledge, there have been no other prior studies comparing catatonia knowledge among psychiatry, internal medicine, and neurology practitioners. Despite the limited sample size of this study, these data do suggest that internists and neurologists interpret catatonic findings differently than psychiatric clinicians. This could be, in part, because of differences in training traditions across specialties, leading to differences in the use of medical nomenclature and terminology.
Given that catatonia often leads to care in an acute medical setting and that it can be the primary presentation of medical and neurological conditions, internists and neurologists would do well to receive instruction on catatonia including what it looks like, its workup, its clinical management, and the importance of collaborating with colleagues in psychiatry.2 One can only speculate regarding what effects the gaps in catatonia knowledge identified in this study have on patient care and clinical outcomes.
We suspect that the modest participation and high attrition rate, despite nearly all subjects’ affirming the importance of catatonia to their specialty and their practice, reflect overall attitudes about catatonia among these specialties. Only 18% of those who consented and met inclusion criteria completed all prelearning module and learning module components. Curiously, those who agreed that catatonia was important to their specialty and clinical practice were not more likely to complete the free catatonia training module. The raffle was also an inadequate incentive for most participants to complete all components of this study.
Our study has multiple strengths. To our knowledge, this is the first study to survey both knowledge of and attitudes toward catatonia among internal medicine and neurology practitioners. Our knowledge assessment builds on our prior work and offered participants training resources that have been shown to improve accuracy in catatonia recognition.11 We also compare current results with those from a prior study among psychiatry practitioners,11 which highlights the need for specialty specific efforts on catatonia education and awareness.
Study limitations include the modest sample size and high attrition rate. Additionally, our study did not ask participants about second-line treatments for catatonia. We attempted to recruit participants using several means. The X/Twitter posts alone received more than 25,000 impressions. Despite widespread dissemination, only 99 completed the online consent form, which may reflect overall attitudes toward catatonia among these specialties. We also suspect that those who chose to participate were likely more interested in and, as a result, more knowledgeable about catatonia, thereby enriching our sample with a higher catatonia knowledge quotient than the average internal medicine or neurology practitioner. However, if this is true, this only magnifies the importance of the gaps we identified. We also acknowledge that the standardized test patient video illustrated only one manifestation of catatonia, which introduces a bias in terms of catatonia item selection. It is also uncertain how well scoring this video translates into clinical practice, where clinicians would need to evaluate for catatonic findings deliberately.
Our results call for efforts on catatonia education and awareness among internists and neurologists. For instance, it would be valuable to replicate these findings in a larger study cohort. The fact that the invitation referred to an hour-long study may have discouraged many from participating, so a brief study that only evaluates participants’ knowledge and impressions might yield a larger cohort. A mixed-methods study that includes narrative responses, structured interviews, or focus groups among internal medicine and neurology practitioners is likely to yield a more nuanced appreciation of impressions and potential areas for needed education and awareness. Although we attempted to evaluate the effect of the learning module on catatonia-related knowledge among internists and neurologists, we were unable to do so due to attrition. Further, evaluating attitudes and knowledge among emergency medicine practitioners, who are often the first point of contact for patients with catatonia, also deserves investigation.
Ultimately, although participants correctly identified medical sequelae of catatonia and benzodiazepines as its first line treatment, gaps in catatonia-related knowledge were identified among internal medicine and neurology practitioners, especially in terms of correctly identifying its individual features. We hope that our results stimulate interest in catatonia among internal medicine and neurology practitioners and that they encourage calls for broader catatonia education and awareness across specialties.
Article Information
Published Online: April 17, 2025. https://doi.org/10.4088/PCC.24m03853
© 2025 Physicians Postgraduate Press, Inc.
Submitted: September 17, 2024; accepted January 7, 2025.
To Cite: Kaur J, Maeng DD, Wortzel JR, et al. What internists and neurologists know and think about catatonia. Prim Care Companion CNS Disord 2025;27(2):24m03853.
Author Affiliations: Department of Psychiatry, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania (Kaur); Department of Psychiatry, University of Rochester Medical Center, Rochester, New York (Maeng, Oldham); Department of Psychiatry, Yale University, New Haven, Connecticut; Hartford HealthCare, Harford, Connecticut (Wortzel).
Corresponding Author: Japsimran Kaur, MD, Department of Psychiatry, University of Pittsburgh Medical Center, 3811 O’Hara St, Pittsburgh, Pennsylvania 15213 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Acknowledgments: The authors wish to thank study partners who helped disseminate the invitation to participate within their networks. The authors are indebted to Andrew Auerbach, MD, MPH (Hospital Medicine ReEngineering Network [HOMERuN] listserv); Megan Richie, MD and Sara LaHue, MD (dissemination via the NeuroHospitalist Society newsletter); Benjamin Kalivas, MD (Society of Hospital Medicine HRX group posts); Christopher Tarolli, MD (American Academy of Neurology’s Synapse message board posts); Michael Okun, MD and Jennifer Readlynn, MD (Twitter/X posts); and Amy Blatt, MD, Valerie Lang, MD, MHPE, and Jospeh Nicholas, MD, MPH (solicitation of internal medicine residents, hospitalists, and geriatricians at the authors’ institution). The authors also acknowledge Hochang B. Lee, MD, without whose support this project would not have been possible. The acknowledged individuals report no conflicts of interest related to the subject of this article.
ORCID: Japsimran Kaur: https://orcid.org/0000-0002-9863-5973; Daniel D. Maeng: https://orcid.org/0000-0002-1867-6629; Joshua R. Wortzel: https://orcid.org/0000-0001-5106-0802; Mark A. Oldham: https://orcid.org/0000-0002-0981-7522
Clinical Points
- Catatonia can be the primary presentation of medical and neurological conditions; prompt recognition and treatment planning is imperative.
- Internal medicine and neurology providers correctly identified catatonia sequelae and benzodiazepines as first-line treatment.
- Gaps in knowledge are most prominent in identifying individual catatonia features; educational resources reviewing these features are available.
References (12)

- Walther S, Strik W. Catatonia. CNS Spectr. 2016;21(4):341–348.
- Rogers JP, Oldham MA, Fricchione G, et al. Evidence-based consensus guidelines for the management of catatonia: recommendations from the British Association for Psychopharmacology. J Psychopharmacol. 2023;37(4):327–369. CrossRef
- Wilson JE, Carlson R, Duggan MC, et al. Delirium and catatonia in critically ill patients: the delirium and catatonia prospective cohort investigation. Crit Care Med. 2017;45(11):1837–1844. CrossRef
- Solmi M, Pigato GG, Roiter B, et al. Prevalence of catatonia and its moderators in clinical samples: results from a meta-analysis and meta-regression analysis. Schizophr Bull. 2018;44(5):1133–1150. CrossRef
- Oldham MA. The probability that catatonia in the hospital has a medical cause and the relative proportions of its causes: a systematic review. Psychosomatics. 2018;59(4):333–340. CrossRef
- van der Heijden FMMA, Tuinier S, Arts NJM, et al. Catatonia: disappeared or under-diagnosed? Psychopathology. 2005;38(1):3–8. CrossRef
- Ghaziuddin N, Dhossche D, Marcotte K. Retrospective chart review of catatonia in child and adolescent psychiatric patients. Acta Psychiatr Scand. 2012;125(1):33–38. CrossRef
- Anand S, Kumar Paliwal V, Singh LS, et al. Why do neurologists miss catatonia in neurology emergency? A case series and brief literature review. Clin Neurol Neurosurg. 2019;184:105375. CrossRef
- Bush G, Fink M, Petrides G, et al. Catatonia. I. Rating scale and standardized examination. Acta Psychiatr Scand. 1996;93(2):129–136. CrossRef
- Wortzel JR, Maeng DD, Francis A, et al. Evaluating the effectiveness of an educational module for the bush-francis catatonia rating scale. Acad Psychiatry. 2022;46(2):185–193. CrossRef
- Wortzel JR, Maeng DD, Francis A, et al. Prevalent gaps in understanding the features of catatonia among psychiatrists, psychiatry trainees, and medical students. J Clin Psychiatry. 2021;82(5):21m14025.
- Cooper JJ, Roig Llesuy J. Catatonia education: needs assessment and brief online intervention. Acad Psychiatry. 2017;41(3):360–363. CrossRef
Enjoy this premium PDF as part of your membership benefits!