Abstract
Objective: To explore depression prevalence, correlates, impact, and interventions in breast cancer patients, with a focus on the Indian context.
Data Sources: The search specifically targeted PubMed as the primary electronic database using keywords such as breast cancer, depression, and India. No date limits were imposed, and studies were restricted to those available in English.
Study Selection: A total of 12 studies were reviewed, comprising original research articles and case studies. Inclusion criteria encompassed studies investigating depression in breast cancer patients, irrespective of study design or intervention type.
Data Extraction: Data abstraction followed predefined guidelines, focusing on depression prevalence rates, factors associated with depression onset, intervention efficacy, and implications for clinical practice. Data were extracted independently by 2 reviewers, with discrepancies resolved through discussion.
Data Synthesis: Findings revealed diverse depression rates among breast cancer patients, ranging from 21.5% to 83.5%. Treatment type, body image concerns postsurgery, stigma, and sociodemographic factors such as low income, education, and rural residency were identified as contributors to depression onset. Nonpharmacologic interventions, particularly yoga and supportive psychotherapy, demonstrated efficacy in mitigating depression symptoms.
Conclusions: This review underscores the multifaceted nature of depression in breast cancer patients and the importance of tailored interventions to address this psychological comorbidity. Integration of mental health services into cancer care frameworks, alongside traditional treatment modalities, is essential to ensure comprehensive support for breast cancer patients. The findings advocate for a holistic approach to mental health within cancer care, emphasizing the need for policy initiatives that prioritize psychosocial well being alongside physical health outcomes.
Prim Care Companion CNS Disord 2024;26(5):24r03721
Author affiliations are listed at the end of this article.
Cancer is a formidable and potentially fatal illness, posing various risks to patients due to the diagnosis of a life-threatening condition, intricate treatment procedures, and subsequent side effects. Consequently, cancer is commonly associated with considerable stress among patients.1,2 Among women worldwide, breast cancer stands as the most prevalent malignancy, surpassing lung cancer in 2020 to become the primary cause of global cancer incidence, accounting for an estimated 2.3 million new cases, and constituting 11.7% of all cancer instances.3 Epidemiologic studies project the global burden of breast cancer to approach nearly 2 million cases by 2030.4
Breast cancer is the most frequently diagnosed cancer among Indian women.5 Recent trends highlight a higher incidence occurring at younger ages in Indian women compared to their Western counterparts. The National Cancer Registry Program analyzed data from 1988 to 2013, revealing a significant upward trend in breast cancer incidence across all population-based cancer registries.5,6 Breast cancer has undergone extensive scrutiny from various perspectives, encompassing clinic epidemiologic, experimental, molecular, and psychological standpoints.7
The diagnosis of cancer affects individuals differently, with emotional and psychological consequences being a key focus among breast cancer patients, including those diagnosed, treated, and surviving the disease.8 One prevalent psychiatric comorbidity observed in this population is depression. This scoping review aims to determine the prevalence of depression, explore its correlations, and assess its multifaceted impacts on breast cancer patients.
METHODS
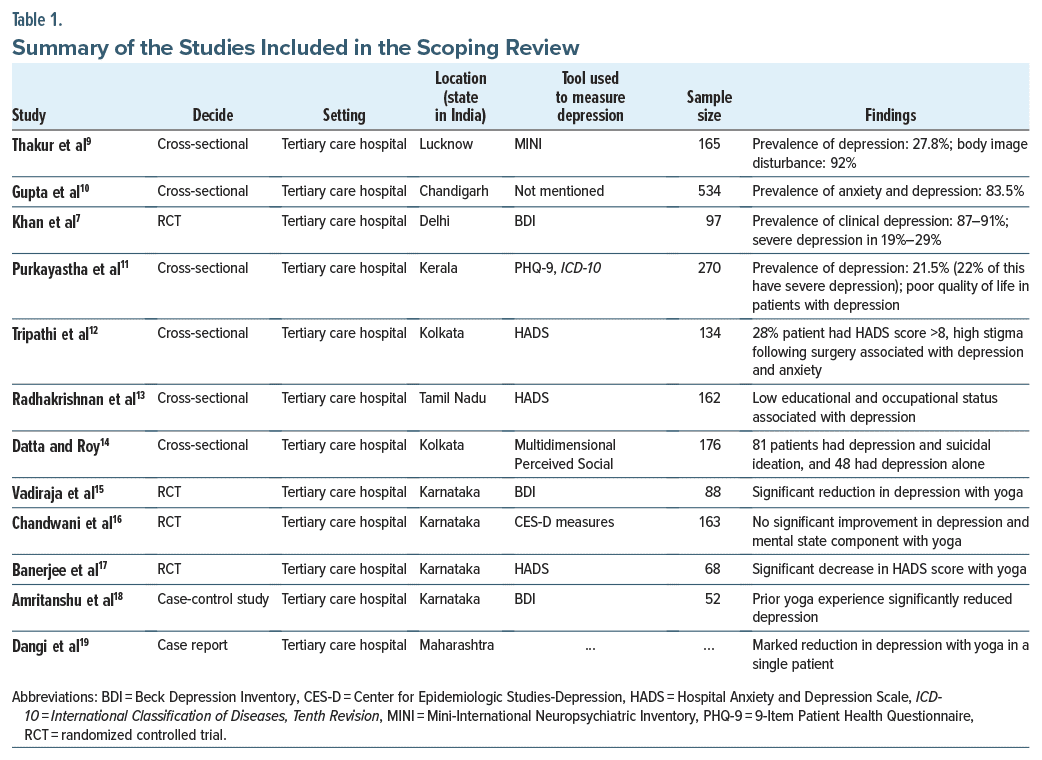
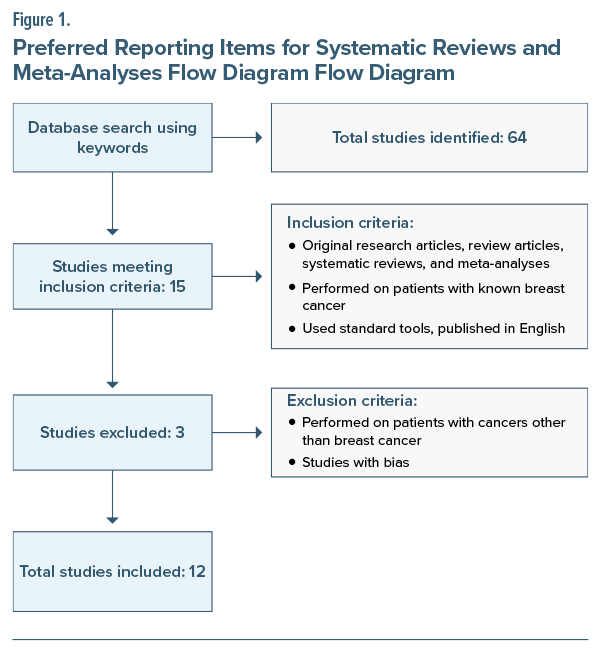
This scoping review focused on the existing research literature published in India. The survey specifically targeted PubMed as the primary electronic database. The search employed keywords such as breast cancer, depression, and India. Only empirical investigations were considered for inclusion in this scoping review. The criteria included studies conducted solely among Indian women with breast cancer and published in English, resulting in the exclusion of several articles that were theoretical, overviews, clinical guidelines, or general observations. This methodological approach led to the identification of 12 relevant articles out of a total of 64 studies retrieved from the database spanning the years 1981–2023. The details of the studies are summarized in Table 1. It is important to note that while this review provides a comprehensive scoping review, it does not aim to offer either an exhaustive coverage or an in-depth analysis of all studies conducted in this field within India. Selection of reviewed articles was done using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram (Figure 1).20
RESULTS
The analysis encompassed 12 articles delving into depression within the context of breast cancer. Among these studies, only 3 (25%) explored the prevalence of depression among breast cancer patients, each with a distinct patient population. Thakur et al9 examined depression prevalence among survivors of breast cancer who underwent modified radical mastectomy. Purkayastha et al11 investigated depression prevalence and its correlation with quality of life (QoL) among breast cancer patients undergoing various treatments. Radhakrishnan et al13 studied depression prevalence in cancer patients irrespective of disease stage. These studies were conducted in tertiary care hospital settings using different depression assessment scales. Another study investigated the impact of different breast cancer treatments on depression prevalence. Khan et al7 demonstrated a higher prevalence of depression among patients undergoing both postoperative adjuvant chemotherapy and radiotherapy compared to those receiving chemotherapy alone (51.51% vs 48.38%).
Two studies10,11 explored QoL among breast cancer patients and identified depression as a significant negative influencer of QoL. One study12 examined stigma and its correlates among breast cancer patients’ postsurgery, revealing depression’s impact on stigma levels. Another study14 explored the association between depression and suicidal thoughts among breast cancer patients.
Five studies (41.67%) investigated the impact of yoga in breast cancer patients at various stages of illness. Vadiraja et al15 assessed the impact of an integrated yoga program combined with brief supportive therapy in breast cancer outpatients receiving adjuvant radiotherapy. Chandwani et al16 examined yoga’s impact on women undergoing radiotherapy for breast cancer using a randomized controlled design. Banerjee et al17 investigated the effects of yoga on perceived stress levels, anxiety, depression, and radiation-induced DNA damage in breast cancer patients undergoing radiotherapy. Amritanshu et al18 explored the long-term effects of yoga practice on psychological outcomes in breast cancer survivors through a case-control study design. Finally, Dangi et al19 reported on the impact of a structured yoga program on fatigue, depression, cardiorespiratory fitness, and QoL in postmenopausal breast cancer survivors. These findings provide insights into the diverse research landscape surrounding breast cancer, shedding light on various psychological, social, and therapeutic aspects of the disease.
Prevalence of Depression in Breast Cancer
Although numerous studies have attempted to explore the relationship between depression and breast cancer, only 4 studies7,9–11 have directly assessed the prevalence of depression among breast cancer patients in India. These studies reported prevalence rates of 27.8%, 83.5%, 87%–91%, and 21.5%, respectively.7,9–11 The most commonly utilized assessment tools for measuring depression were the Hospital Anxiety and Depression Scale (HADS), along with other tools such as the Mini-International Neuropsychiatric Interview, Beck Depression Inventory, and International Classification of Diseases, Tenth Revision. Among the identified studies, research conducted in a single institute in South India assessed depression and anxiety across various cancer types and found a higher prevalence of depression among breast cancer and gastrointestinal cancer patients.13
Correlates and Impact of Depression in Breast Cancer
Several studies have delved into the correlates of depression among breast cancer patients. A cross sectional study9 conducted among 165 female breast cancer survivors from a north Indian tertiary care center aimed to explore the psychological impact of modified radical mastectomy surgery. The study revealed that 27.8% of patients experienced depression, with 92% reporting body image disturbances within the initial period (less than 12 months) postsurgery. Additionally, 31.5% experienced anxiety, and 24.8% reported stress.9
Another study7 conducted in Delhi, India assessed behavioral and psychosocial impacts before and after treatment in women with breast cancer and found that 19%–29% of patients suffered from severe depression and 39% experienced borderline depression. Although sociobehavioral disorders were more prevalent in patients undergoing postoperative adjuvant chemotherapy and radiotherapy than in those on postoperative adjuvant chemotherapy alone, this disparity was not statistically significant.7
A comprehensive cancer center study12 involving 134 women highlighted a correlation between high stigma levels and increased depression and anxiety among patients undergoing surgical treatment for breast cancer. Stigma was measured using the Body Image after Breast Cancer questionnaire, while depression was assessed using the depression subscale of the HADS. The results revealed that stigma was significantly associated with depression, showing a relationship in which those experiencing depression were more likely to encounter higher levels of stigma. This finding suggests a bidirectional relationship between stigma and depression, wherein higher stigma may contribute to or exacerbate depressive symptoms.12
Two studies explored the correlation of sociodemographic variables in cancer patients, with a majority being breast cancer patients. One study10 associated low educational and occupational status with higher depression in breast cancer patients, highlighting that breast cancer significantly elevates the risk of depression. Another study14 found that various factors studied, including low educational status, rural residency, and low income, significantly impacted depression, anxiety, and overall QoL in cancer patients.
Furthermore, 2 studies investigated the impact of depression on breast cancer patients. A study from Kerala involving 270 diagnosed breast cancer patients discovered a lower overall QoL among patients with depression, showcasing a positive association between depression and various domains of QoL. Patients with depression scored lower across all domains compared to those without depression.11
In another study involving 176 breast cancer patients, 81 exhibited suicidal thoughts in addition to depression, while 48 displayed depression without suicidal ideation. Suicidal ideation was linked to impaired social emotion recognition and social support, hindering patients’ ability to seek adequate social support.14
Interventions Employed for Managing Depression in Breast Cancer Patients
Two studies aimed at assessing the impact of yoga compared to other interventions, such as supportive psychotherapy or stretching, revealed varying outcomes in managing depression among breast cancer patients. One study15 involving a 24-week integrated yoga program reported a significant reduction in depression scores compared to a control group receiving supportive psychotherapy during conventional breast cancer treatment. Conversely, another study16 employing a 6-week yoga program during radiotherapy yielded no significant variations in depression scores. However, the yoga group exhibited notably increased physical well-being compared to the waitlisted patients, possibly attributed to the program’s short duration and ongoing stressors.16 Additional investigations revealed reductions in depression and anxiety among early-stage breast cancer patients undergoing adjuvant therapy following yoga sessions.17 Moreover, integrated yoga programs significantly reduced depression and anxiety scores in patients undergoing breast cancer radiotherapy.19 A case control study18 explored the impact of long-term yoga practice on predicting depression and found that prior yoga experience was associated with lower stress, depression, and anxiety levels, indicating a potential benefit for individuals with a history of regular yoga practice after completing cancer treatment. Furthermore, a case report19 involving a postmenopausal breast cancer survivor undergoing a structured yoga program 5 times a week for 4 weeks demonstrated a marked reduction in depression and fatigue scores, along with improvements in cardiorespiratory fitness and overall QoL.
DISCUSSION
Breast cancer often acts as a significant contributing factor to the onset of depression, with varying prevalence rates observed across different populations. In the Indian population, prevalence rates were reported as 27.8%, 83.5%, 87%–91%, and 21.5%. Conversely, studies conducted in other countries found diverse prevalence rates: 26% in China,21 16.7% in Thailand,22 54.5% in Greece,23 18% in Italy,24 and moderate (11%) to severe (12%) rates in Germany.25 A 5-year cohort study in the United Kingdom indicated a 50% prevalence during the first year of cancer diagnosis, which gradually declined over time.26 Studies in the United States showed varying prevalence rates, ranging from 46% to 56%.27,28 These substantial variations in prevalence might stem from differences in assessment methodologies, demographic factors, cultural and ethnic influences, cancer stage, duration, and the type of treatment received by patients. The utilization of diverse assessment tools for depression could also contribute to variations in study outcomes. Additionally, most studies assessed anxiety concurrently with depression, reporting prevalence rates for the comorbidity of these 2 conditions. This high comorbidity might be attributed to the tools employed for screening depression and anxiety together in breast cancer cases.
The diagnosis of breast cancer is often accompanied by a multitude of psychological stresses. Several factors contribute to these psychological reactions, starting from the moment of diagnosis to the prolonged and uncertain nature of the treatment process.8 Additional contributory factors that may foster anxiety and depression include the fear of an incurable disease, fear of mortality, separation from loved ones, alterations in body image perception, apprehension about pain, the nature of the treatment received, and the patient’s background.8 In this particular study, it was identified that the type of treatment received for breast cancer, postsurgical body image disturbances, the level of stigma, and sociodemographic factors, such as low-income status, limited education, and residing in rural areas, significantly correlate with the development of depression. Similar associations between breast cancer and the type of interventions, such as chemotherapy or therapy, have been reported in studies conducted in other countries.29–31 For instance, a study by Chen et al21 suggested a positive correlation between low-income status and depression.
The management of comorbid depression in breast cancer is crucial for enhancing both the patients’ QoL and their adherence to cancer treatment. In our investigation, we found various studies focused on assessing the efficacy of nonpharmacologic interventions aimed at mitigating depression in breast cancer patients. These interventions primarily encompassed yoga and supportive psychotherapy. However, none of the studies explored the effectiveness of pharmacologic methods or structured psychotherapies. The majority of these studies concluded that yoga exhibits effectiveness in alleviating depression among breast cancer patients, aligning with earlier observations that highlighted the positive impact of yoga in both cancer and noncancer populations.32–35 Literature from the Western world suggests a combination of approaches, including both sequential and integrated strategies, for effectively treating depression in this particular population.36
CONCLUSION
In conclusion, depression prevalence in breast cancer patients varies across studies. Psychological stressors, including disease-related fears, body image changes, and sociodemographic factors, contribute significantly to depression. Managing depression is crucial for patients’ QoL and treatment adherence.
Nonpharmacologic interventions such as yoga and supportive psychotherapy show promise in alleviating depression in breast cancer patients. However, there is a need to explore more treatment options beyond nonpharmacologic approaches. Integrating
comprehensive strategies could improve patient well being and enhance overall cancer care. Further research in this area will be essential for developing holistic approaches to address depression in breast cancer patients effectively.
Article Information
Published Online: September 26, 2024. https://doi.org/10.4088/PCC.24r03721
© 2024 Physicians Postgraduate Press, Inc.
Submitted: February 11, 2024; accepted May 20, 2024.
To Cite: Vaseel M, Uvais NA. Breast cancer and depression: a scoping review of Indian literature. Prim Care Companion CNS Disord. 2024;26(5):24r03721.
Author Affiliation: Department of Psychiatry, Iqraa International Hospital and Research Centre, Calicut, India (all authors).
Corresponding Author: N. A. Uvais, MBBS, DPM, Iqraa International Hospital and Research Centre, Malaparamba 673009, Calicut, Kerala, India ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Previous Presentation: This scoping review was presented as a poster at MIND CAN 2023 “The Art and Science of Closing the Care Gap in Cancer” One Day National Conference on Psycho-Oncology; October 14, 2023; Kannur, India.
Clinical Points
- Depression prevalence in breast cancer patients varies across studies.
- Psychological stressors, including disease-related fears, body image changes, and sociodemographic factors, contribute significantly to depression.
- Depression management is crucial for quality of life and treatment adherence.
References (36)

- Zhang AY, Cooper GS. Recognition of depression and anxiety among elderly colorectal cancer patients. Nurs Res Pract. 2010;2010:693961. PubMed CrossRef
- Tavoli A, Mohagheghi MA, Montazeri A, et al. Anxiety and depression in patients with gastrointestinal cancer: does knowledge of cancer diagnosis matter? BMC Gastroenterol. 2007;7:28. PubMed CrossRef
- Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–249. PubMed CrossRef
- DeSantis C, Siegel R, Bandi P, et al. Breast cancer statistics, 2011. CA Cancer J Clin. 2011;61:409–418. PubMed CrossRef
- National Cancer Registry Programme. Three-Year Report of the Population Based Cancer Registries, 2012–2014. Indian Council of Medical Research; 2016.
- Mehrotra R, Yadav K. Breast cancer in India: present scenario and the challenges ahead. World J Clin Oncol. 2022;13(3):209–218. PubMed CrossRef
- Khan MA, Bahadur AK, Agarwal PN, et al. Psychosocial disorders in women undergoing postoperative radiation and chemotherapy for breast cancer in India. Indian J Cancer. 2010;47(3):296–303. PubMed CrossRef
- Thakur M, Sharma R, Mishra AK, et al. Prevalence and psychobiological correlates of depression among breast cancer patients. Indian J Surg Oncol. 2021;12(2):251–257. PubMed CrossRef
- Thakur M, Sharma R, Mishra AK, et al. Psychological distress and body image disturbances after modified radical mastectomy among breast cancer survivors: a cross-sectional study from a tertiary care centre in North India. Lancet Reg Health Southeast Asia. 2022;7:100077. PubMed CrossRef
- Gupta N, Pandey AK, Dimri K, et al. Health-related quality of life among breast cancer patients in India. Support Care Cancer. 2022;30(12):9983–9990. PubMed CrossRef
- Purkayastha D, Venkateswaran C, Nayar K, et al. Prevalence of depression in breast cancer patients and its association with their quality of life: a cross-sectional observational study. Indian J Palliat Care. 2017;23(3):268–273. PubMed CrossRef
- Tripathi L, Datta SS, Agrawal SK, et al. Stigma perceived by women following surgery for breast cancer. Indian J Med Paediatr Oncol. 2017;38(2):146–152. PubMed CrossRef
- Radhakrishnan R, Selvaraj H, Chidambaram K, et al. Prevalence of depression and anxiety disorders among cancer patients: an insight from a single institute. Cureus. 2023;15(8):e42831. PubMed CrossRef
- Datta A, Roy S. Social emotion recognition, social functioning and suicidal behaviour in breast cancer patients in India. Gulf J Oncolog. 2022;1(39):31–38. PubMed
- Vadiraja HS, Raghavendra RM, Nagarathna R, et al. Effects of a yoga program on cortisol rhythm and mood states in early breast cancer patients undergoing adjuvant radiotherapy: a randomized controlled trial. Integr Cancer Ther. 2009;8(1):37–46. PubMed CrossRef
- Chandwani KD, Perkins G, Nagendra HR, et al. Randomized, controlled trial of yoga in women with breast cancer undergoing radiotherapy. J Clin Oncol. 2014;32(10):1058–1065. PubMed CrossRef
- Banerjee B, Vadiraj HS, Ram A, et al. Effects of an integrated yoga program in modulating psychological stress and radiation-induced genotoxic stress in breast cancer patients undergoing radiotherapy. Integr Cancer Ther. 2007;6(3):242–250. PubMed CrossRef
- Amritanshu RR, Rao RM, Nagaratna R, et al. Effect of long-term yoga practice on psychological outcomes in breast cancer survivors. Indian J Palliat Care. 2017;23(3):231–236. PubMed CrossRef
- Dangi AA, Aurangabadkar SK, Deo MV. Effect of a structured yoga program on fatigue, depression, cardiorespiratory fitness, and quality of life in a postmenopausal breast cancer survivor. Int J Yoga. 2018;11(3):255–257. PubMed CrossRef
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372(71):n71. PubMed CrossRef
- Chen X, Zheng Y, Zheng W, et al. Prevalence of depression and its related factors among Chinese women with breast cancer. Acta Oncol. 2009;48(8):1128–1136. PubMed CrossRef
- Lueboonthavatchai P. Prevalence and psychosocial factors of anxiety and depression in breast cancer patients. J Med Assoc Thai. 2007;90(10):2164–2174. PubMed
- Fradelos EC, Papathanasiou IV, Veneti A, et al. Psychological distress and resilience in women diagnosed with breast cancer in Greece. Asian Pac J Cancer Prev. 2017;18(9):2545–2550. PubMed CrossRef
- Pumo V, Milone G, Iacono M, et al. Psychological and sexual disorders in long term breast cancer survivors. Cancer Manag Res. 2012;4:61–65. PubMed CrossRef
- Mehnert A, Koch U. Psychological comorbidity and health-related quality of life and its association with awareness, utilization, and need for psychosocial support in a cancer register-based sample of long-term breast cancer survivors. J Psychosom Res. 2008;64(4):383–391. PubMed CrossRef
- Burgess C, Cornelius V, Love S, et al. Depression and anxiety in women with early breast cancer: five-year observational cohort study. BMJ. 2005;330(7493):702. PubMed CrossRef
- Christie KM, Meyerowitz BE, Maly RC. Depression and sexual adjustment following breast cancer in low-income Hispanic and non-Hispanic White women. Psychooncology. 2010;19(10):1069–1077. PubMed CrossRef
- Begovic-Juhant A, Chmielewski A, Iwuagwu S, et al. Impact of body image on depression and quality of life among women with breast cancer. J Psychosoc Oncol. 2012;30(4):446–460. PubMed CrossRef
- Morasso G, Costantini M, Viterbori P, et al. Predicting mood disorders in breast cancer patients. Eur J Cancer. 2001;37(2):216–223. PubMed CrossRef
- Onen Sertöz O, Elbi Mete H, Noyan A, et al. [Effects of surgery type on body image, sexuality, self-esteem, and marital adjustment in breast cancer: a controlled study]. Turk Psikiyatri Derg. 2004;15(4):264–275. PubMed
- Dujmović A, Marčinko D, Bulić K, et al. Quality of life and depression among female patients undergoing surgical treatment for breast cancer: a prospective study. Psychiatr Danub. 2017;29(3):345–350.
- Speca M, Carlson LE, Goodey E, et al. A randomized, wait-list controlled clinical trial: the effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosom Med. 2000;62:613–622. PubMed CrossRef
- Brown RP, Gerbarg PL. Sudarshan Kriya Yogic breathing in the treatment of stress, anxiety, and depression: part II—clinical applications and guidelines. J Altern Complement Med. 2005;11:711–717. PubMed CrossRef
- Hidderley M, Holt M. A pilot randomized trial assessing the effects of autogenic training in early stage cancer patients in relation to psychological status and immune system responses. Eur J Oncol Nurs. 2004;8:61–65. PubMed CrossRef
- Danhauer SC, Tooze JA, Farmer DF, et al. Restorative yoga for women with ovarian or breast cancer: findings from a pilot study. J Soc Integr Oncol. 2008;6:47–58. PubMed
- Keller MB, McCullough JP, Klein DN, et al. A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression. N Engl J Med. 2000;342:1462–1470. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!