Catatonia is an acute state marked by psychomotor, neurological, and behavioral changes.1 We present a case of a patient with catatonia and worsening episodes of anxiety, insomnia, and alterations in cognition found to concurrently have autoimmune thyroid disease (AITD). Due to an unremarkable initial workup, accurate diagnosis was challenging. A robust review of the medical causes of catatonia eventually yielded a productive diagnostic workup.
Case Report
A 26-year-old white woman presented to the emergency department (ED) after 5 months of progressively worsening premenstrual and cyclic episodes of anxiety, insomnia, stereotypic movements, disorientation, memory lapses, blurry vision, and anorexia, which led to multiple prior hospitalizations. Blurry vision was intermittent and endorsed specifically during periods of anxiety and insomnia. She denied diplopia or eye pain. Family history was significant for cyst thyroidectomy and Graves disease, as well as nonspecific anxiety and depression. At symptom onset, the patient had an elevated thyroid stimulating hormone (TSH) level of 11.9 mcIU/mL (reference range, 0.5–5.0 mcIU/mL), but repeat laboratory tests showed TSH, T4, and T3 values within normal limits. Workups were negative, including routine blood work, vitamin B12, magnesium, toxicology screens, and antinuclear antibodies. Sleep studies, brain magnetic resonance imaging, computed tomography scan, electroencephalography, cerebrospinal fluid analysis, and infectious workups were also unremarkable. Her diagnosis remained uncertain, and she was repeatedly discharged home after stabilization.
Previous trials of escitalopram, mirtazapine, and trazodone did not improve her condition. Lorazepam and transcranial magnetic stimulation were also trialed and improved symptoms, but treatment was discontinued due to patient reluctance.
She was admitted to the hospital from the ED due to a sharp decline in functional status. She displayed mutism, poor eye contact, agitation, and significant paranoia with persecutory delusions and was treated with olanzapine. The physical examination was negative for ophthalmopathy. She displayed subtle signs of echopraxia, so further evaluation of catatonia was performed with the patient scoring a 19 on the Bush-Francis Catatonia Rating Scale (BFCRS).2 Lorazepam challenge was administered with positive response. Lorazepam 0.5 mg intravenous 3 times daily was initiated, and olanzapine was discontinued. Lorazepam was subsequently titrated to response and switched to oral route. Symptoms improved substantially, confirming catatonia. Lamotrigine was given for suspicion of underlying bipolar disorder but was discontinued due to temporally associated transaminitis. Given the initial TSH abnormality, antithyroid peroxidase antibody was obtained and found to be elevated at 963 IU/mL (reference range, 0–9 IU/mL), suggesting Hashimoto thyroiditis. Due to medical stability, she was discharged home with lorazepam and endocrine follow up.
Postdischarge, under continued lorazepam treatment, endocrinology evaluated thyroid-stimulating immunoglobulin (TSI), a subtype of TSH receptor antibody. The patient’s TSI was elevated at 1.76 IU/L (reference range, ≤0.56 IU/L), which approaches 100% specificity for Graves hyperthyroidism3 and is only simultaneously seen in 10%–15% of those with Hashimoto thyroiditis.4 Due to normal thyroid hormone levels and lack of gross ophthalmopathy, no treatments for Graves disease were initiated, and she was scheduled for frequent follow-up and laboratory monitoring.
Discussion
This case demonstrates an example of AITD-induced catatonia when multiple previous medical workups were unrevealing. AITD creates antibodies against the thyroid gland, leading to respective antibody sequelae: hyperthyroid, neutral, or hypothyroid state.4,5 Psychomotor manifestations such as psychosis, mania, depression, dementia, and catatonia4 have all been described in AITD. Previous studies suggest psychiatric symptoms resolve when abnormal thyroid function is treated.6,7 We expect the patient’s episodes to subside with appropriate management.
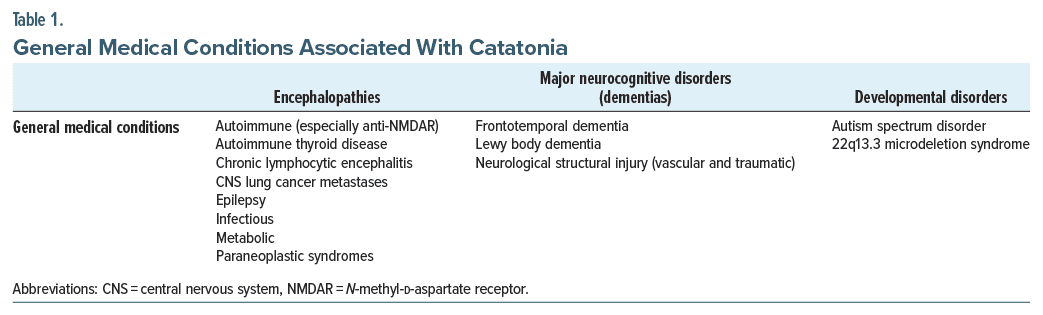
Diagnosis of catatonia incorporates 3 or more of any 12 DSM-5 criteria, 1 qualitative scaling by BFCRS,2 and evaluation for underlying causality.8,9 While psychotic and major mood disorders classically explain a sizable portion of catatonia, the DSM-5 now acknowledges medical causes (Table 1).1,8,10 In the absence of clear psychological diagnosis, etiology must be established in each catatonic patient for proper treatment to counteract catatonia reoccurrence9 or exacerbation of symptoms.
Our patient presented with AITD induced catatonia in the absence of compelling workup. This case demonstrates why physicians should keep a broad medical differential in patients with acute catatonic states.
Article Information
Published Online: October 17, 2024. https://doi.org/10.4088/PCC.24cr03762
© 2024 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2024;26(5):24cr03762
Submitted: April 29, 2024; accepted July 23, 2024.
To Cite: Nawojski SV, Judah ML, Kelly GL, et al. Autoimmune thyroid disease–induced catatonia with normal thyroid function. Prim Care Companion CNS Disord. 2024;26(5):24cr03762.
Author Affiliations: College of Medicine, University of Nebraska Medical Center, Omaha, Nebraska (Nawojski, Judah, Kelly); Department of Psychiatry, University of Nebraska Medical Center, Omaha, Nebraska (Sharma, Reihe).
Corresponding Author: Casey A. Reihe, MD, Department of Psychiatry, University of Nebraska Medical Center, 619 S 42nd St, Omaha, NE 68198 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Consent was received to publish the case report, and information has been de-identified to protect anonymity.
References (10)

- Tandon R, Heckers S, Bustillo J, et al. Catatonia in DSM-5. Schizophr Res. 2013;150(1):26–30. PubMed
- Bush G, Fink M, Petrides G, et al. Catatonia. I. Rating scale and standardized examination. Acta Psychiatr Scand. 1996;93(2):129–136. PubMed CrossRef
- Barbesino G, Tomer Y. Clinical review: clinical utility of TSH receptor antibodies. J Clin Endocrinol Metab. 2013;98(6):2247–2255. PubMed CrossRef
- Loscalzo J, Fauci A, Kasper D. Harrison’s Principles of Internal Medicine, 21e. McGraw Hill Medical. Accessed March 28, 2024. https://accessmedicine.mhmedical.com/book.aspx?bookId=3095
- Fröhlich E, Wahl R. Thyroid autoimmunity: role of anti thyroid antibodies in thyroid and extra-thyroidal diseases. Front Immunol. 2017;8:521. PubMed
- Ransing RS, Mishra KK, Sarkar D. Neuropsychiatric manifestation of hashimoto’s encephalopathy in an adolescent and treatment. Indian J Psychol Med. 2016;38(4):357–360. PubMed CrossRef
- Johnson ET, Eraly SG, Aandi Subramaniyam B, et al. Complexities of cooccurrence of catatonia and autoimmune thyroiditis in bipolar disorder: a case series and selective review. Brain Behav Immun Health. 2022;22:100440. PubMed CrossRef
- Rogers JP, Zandi MS, David AS. The diagnosis and treatment of catatonia. Clin Med (Lond). 2023;23(3):242–245. PubMed
- Walther S, Stegmayer K, Wilson JE, et al. Structure and neural mechanisms of catatonia. Lancet Psychiatry. 2019;6(7):610–619. PubMed CrossRef
- Smith JH, Smith VD, Philbrick KL, et al. Catatonic disorder due to a general medical or psychiatric condition. J Neuropsychiatry Clin Neurosci. 2012;24(2):198–207. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!