Avoidant-restrictive food intake disorder (ARFID) was introduced as a new feeding and eating disorder in the DSM-51 and ICD-11.2 ARFID is characterized by avoidant or restrictive eating in 1 or more of the following: (1) significant weight loss or failure to achieve expected weight gain, (2) nutritional deficiency, (3) dependence on enteral feeding or oral nutritional supplements, and (4) interference with psychosocial functioning.
It differs from other eating disorders in the absence of fear of gaining weight or body image distortions. The DSM-5 describes 3 subtypes of ARFID presentations: avoidance based on sensory characteristics of food, fear of aversive consequences associated with the food, and lack of interest in eating. Though it has been classically thought to be a childhood disorder, ARFID has been increasingly recognized in the adult population as well. Studies have shown that most cases of childhood ARFID, if untreated, persist into adulthood. The point prevalence of adult ARFID is 0.8% for women and 0.9% for men.3 A few studies, mostly from the West, have examined ARFID symptomatology in the adult population and found fear of aversive consequences of food, comorbid anxiety, and depression with significant quality of life impairment to be most common.4,5 The treatment strategies described for childhood ARFID, including family-parent intervention,6 do not work with the adult population, and specific psychological treatment needs to be devised depending on the age group and subtype of ARFID. Here, we present the case of an adult patient with ARFID and comorbid depression.
Case Report
Ms A, a 24-year-old unmarried woman pursuing her postgraduate degree, was temperamentally slow to warm up with anxious-avoidant and obsessive-compulsive personality traits. She had a medical history of irregular menstrual cycles, with a family history of depression in her brother and schizophrenia, obsessive-compulsive disorder, and depression in her paternal grandmother. She presented in April 2022 with an illness duration of 7 years, episodic in course; the first episode was in 2015—moderate depressive episode without somatic syndrome lasting for around 2 months with partial interepisodic recovery (no treatment). The current episode had persisted for the past 2 years and was insidious in onset and continuous in course, with symptoms suggestive of recurrent depressive disorder, moderate depressive episode with somatic syndrome, generalized anxiety disorder, and cluster C personality traits (anxious-avoidant and obsessive compulsive personality traits).
Ms A had peculiar patterns of eating noted since 3 to 4 years of age, which were gradually progressive with worsening since puberty and subsequent fluctuations during increasing stressors and depressive episodes. She had absent parenting in her childhood due to her brother’s illness. Her mother and father were from different cultural backgrounds with differences in their culinary heritage and day-to-day meals. When she was around 3 years of age, her brother was born, and he was diagnosed with retinoblastoma of the right eye. Her mother was busy managing his treatment and surgery, so she was mostly taken to her paternal grandparents’ house against her wishes. She did not like being there or the food given. She missed her mother, and her father would not pay much attention to her during this time. So, her mother had to change the meals to satisfy her and would have to be with her when she ate.
Whenever Ms A would eat out, the smell, texture, and appearance of the food mattered. She preferred to eat the same thing again and again, as she was sure of what to expect from the food. She would avoid food based on sensory characteristics of texture, smell, and appearance. In her words, the tomatoes smelled bad and had a gooey texture from the inside, the watermelon had black seeds in it, carrots were hard to bite and would feel raw, the texture of lettuce was not good, broccoli looked scary, apples had an unpredictable texture from inside, pears looked weird and smelled different, cherries were sour in taste, and strawberries had weird seeds outside and could be sour. Grapes could be sour, and she was scared to experiment; guava had seeds inside; she hated how jackfruit looked from the outside with the spiky pointy texture; somebody once said that sugar cane could cut the tongue; eggplant looked scary from the inside; chilies were spicy; and peas tasted awful. She hated chopped pieces of raw ginger because of smell and taste; bottle gourd had a slimy texture after cooking; baby corn was hard to bite; and butter was salty. She also mentioned that she did not like drinking water, as it had a weird taste.
She used to enjoy the food cooked at home, and there was always a specific routine regarding food. Whenever she would go out, she would always choose dishes that she knew were safe. She would hesitate to try new dishes but sometimes would do so when the food smelled or looked good. She would also avoid going out with friends, as she was unsure of having to eat food that she was uncomfortable with, and at times would just not order and be satisfied with water. She would feel weak most of the time, but her appetite was still reduced. There was significant weight loss with marked interference in psychosocial functioning. Previous weight records were unavailable, but she mentioned she had never weighed more than 40 kg (88 lb) so far. There was no regurgitation of food or any episode of choking in the past. There was no history of improvement of appetite with improvement in mood.
Treatment Progress. The patient was admitted to the hospital given her poor oral intake, and tablet escitalopram was started up to 15 mg. Her baseline body mass index (BMI) was 12.19 kg/m2, and her Hamilton Depression Rating Scale7 (HDRS) score was 22. Intake output charting was started, and daily weight monitoring was done. Individual therapy was started, initially focusing on her mood and slowly evading into her eating habits and beliefs. Therapy sessions were initiated to address concerns related to ARFID with an eclectic approach. The focus of the sessions was on exploring and understanding Ms A’s relationship with food, identifying specific triggers and developing strategies to improve her eating habits and overall nutritional well-being. Also, through exploration and reflection, improvement in her social relationships was attempted. The patient reported ongoing challenges with a limited and selective diet, expressing difficulties in trying new foods and experiencing anxiety around certain textures, tastes, and smells. She also expressed that these challenges had negatively impacted her overall quality of life, social relationships, and physical health.
Initial sessions were focused on rapport building and establishing a therapeutic alliance. In-depth clarifications were made about her childhood history, family environments, and premorbid personality. Uncertainty and ambiguity in the immediate surroundings in childhood, with her father being blind and high achieving, obsessive compulsive, and rigid, reinforced a perceived high expectation of self and perfectionism. Her family imposed the same high expectations and an elevated sense of responsibility, as they were rigid and obsessive regarding academics, food, and other choices. Difficulties in exploring new avenues including food were also noted. Her main difficulty was with the food groups that included fruits, vegetables, and meat. She reported feeling an aversion to these food items, as she was unclear about their origin and could not understand how they could turn into food.
Psychoeducation was initiated with normalization of the existing eating patterns and discussion of the nutritional aspects of food and the need for a balanced diet. A framework of an eating disorder with the perpetuating factors was also explained. The curves of anxiety for neutralization and habituation were explained.
Cognitive distortions were elicited during the sessions—all or none thinking, catastrophizing, overgeneralization, jumping to conclusions, elevated sense of responsibility, and personalization. Restructuring of the cognitive distortions was attempted during the sessions. Negative thoughts and beliefs related to food were elicited and challenged, while collaboratively working on reframing unhelpful thinking patterns and fostering a more positive relationship with food.
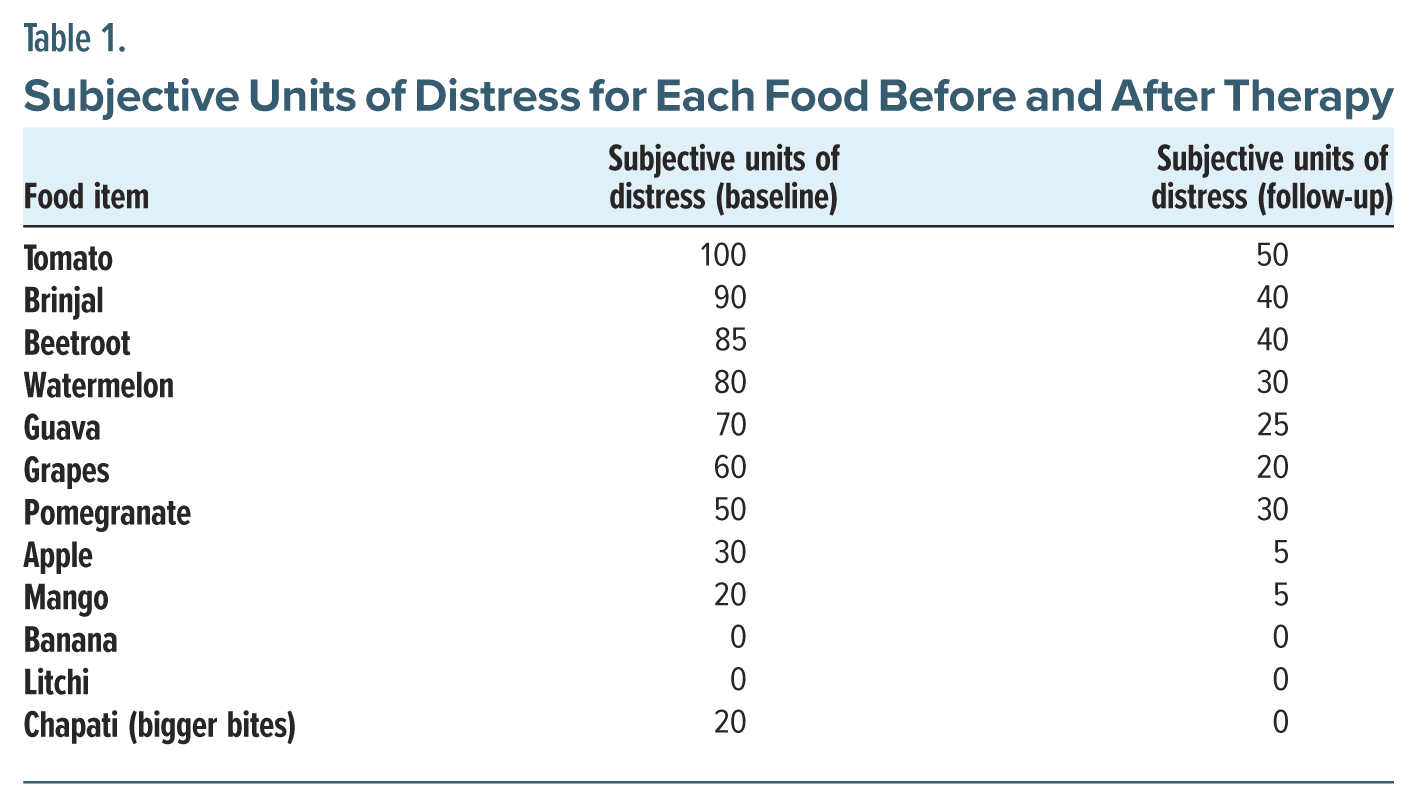
A list of what she called “safe” and “unsafe” meals was made, and a gradual fear hierarchy was established with the patient, mainly incorporating fruits and vegetables. Relaxation exercises were used to help the patient cope with anxiety. Gradual exposure, which was therapist-assisted, involved increasing the amount and variety of food. She was encouraged to take bigger bites and to eat more rapidly with each session. She was encouraged to try new items, slowly and gradually, always respecting her difficulties. At each visit, it was suggested that she experience the food and feel its texture since she was also uncomfortable handling some food items. Then, she was encouraged to smell the food item, put it in her mouth, chew it, and finally swallow it. She was instructed to complete each of these steps whenever she tried new foods, taking as much time as she needed to feel comfortable. She was encouraged to choose the food item of her choice for in vivo sessions. Ms A was asked to rate her anxiety for each session on a scale of 0–100. At first, the patient wanted to stop eating after taking a few bites, as she felt full or uneasy; however, once the level of uneasiness subsided, she was instructed to resume eating later. Her anxiety decreased gradually with each session. She was also given tasks to be done at home, and a log of the tasks was kept with the maintenance of a food diary. Table 1 provides subjective units of distress for each food pre- and posttherapy.
A gradual improvement in the subjective units of distress was noted with the incorporation of the same techniques in daily meals. A track of her meals and water intake was also done during therapy sessions. Mindfulness techniques were introduced to enhance awareness of hunger and fullness cues, as well as the sensory experience of eating, and she was encouraged to approach meals with curiosity and openness.
She was followed up with a plan of weekly therapy sessions for 6 months after discharge. She gained 8 kg (17 lb), reaching a BMI of 15.26 kg/m2 and a HDRS score of 2. With the improvement noted in overall mood and eating patterns, the frequency of sessions was gradually decreased to twice a month and then once a month, and booster sessions are currently ongoing once every 3 months at the time of this writing. She continues to have monthly follow-up appointments with the treating team and can eat 3 meals a day and finish nearly 80% of her meals, compared with 20% when she first presented. She also reported that going out with friends was easier than before.
Conclusion
Our patient had onset of ARFID in childhood, which had continued into adulthood. She mainly had concerns regarding the sensory characteristics of the food and did not have a lack of interest in eating or aversive consequences regarding food. This is the least-studied subtype of ARFID, as it is less common in children and adolescents.8 Her symptoms of ARFID had a chronic course with fluctuations during the depressive episodes. Though her depressive symptoms improved with escitalopram, ARFID symptoms persisted. Hence, individual therapy was started focusing mainly on ARFID. An eclectic approach was taken, incorporating principles from supportive, cognitive behavioral, and mindfulness therapy. Improvement was noted in food intake and BMI after several behavioral exposure sessions. As there are no treatment guidelines yet for ARFID in adults, individualized approaches would help to understand different presentations and treatment responses, as well as inform protocols.
Article Information
Published Online: March 4, 2025. https://doi.org/10.4088/PCC.24cr03811
© 2025 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2025;27(2):24cr03811
Submitted: July 10, 2024; accepted December 7, 2024.
To Cite: Praveen AP, Chithra NK, Jayasankar P, et al. Clinical presentation and treatment challenges in adult avoidant-restrictive food intake disorder. Prim Care Companion CNS Disord 2025;27(2):24cr03811
Author Affiliations: National Institute of Mental Health and Neurosciences, Bengaluru, India (Praveen); Department of Psychiatry, University of British Columbia, Vancouver, British Columbia (Chithra); Centre for Brain and Mind, National Institute of Mental Health and Neurosciences, Bengaluru, India (Jayasankar); Department of Psychiatry, National Institute of Mental Health and Neurosciences, Bengaluru, India (Jayasankar, Kumar K G).
Corresponding Author: Pavithra Jayasankar, MD, Department of Psychiatry, Centre for Brain and Mind, National Institute of Mental Health and Neurosciences, Bengaluru 560029, India ([email protected]m).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Consent was received from the patient to publish the case report, and information, including dates, has been de-identified to protect anonymity.
References (8)

- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
- International Classification of Diseases, Eleventh Revision (ICD-11). World Health Organization (WHO); 2019/2021. Accessed November 7, 2024. https://icd.who.int/browse11.
- Hilbert A, Zenger M, Eichler J, et al. Psychometric evaluation of the Eating Disorders in Youth Questionnaire when used in adults: prevalence estimates for symptoms of avoidant/restrictive food intake disorder and population norms. Int J Eat Disord. 2021;54(3):399–408. PubMed CrossRef
- Zickgraf HF, Franklin ME, Rozin P. Adult picky eaters with symptoms of avoidant/restrictive food intake disorder: comparable distress and comorbidity but different eating behaviors compared to those with disordered eating symptoms. J Eat Disord. 2016;4:26. PubMed CrossRef
- Manwaring JL, Blalock DV, Rienecke RD, et al. A descriptive study of treatment-seeking adults with avoidant/restrictive food intake disorder at residential and inpatient levels of care. Eat Disord. 2024;32(1):13–28. PubMed CrossRef
- Rienecke RD, Drayton A, Richmond RL, et al. Adapting treatment in an eating disorder program to meet the needs of patients with ARFID: three case reports. Clin Child Psychol Psychiatry. 2020;25(2):293–303. PubMed CrossRef
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23(1):56–62. CrossRef
- Katzman DK, Guimond T, Spettigue W, et al. Classification of children and adolescents with avoidant/restrictive food intake disorder. Pediatrics. 2022;150(3):e2022057494. PubMed
Enjoy this premium PDF as part of your membership benefits!