Clozapine is often prescribed to manage treatment-resistant schizophrenia,1,2 defined as an inadequate response to at least 2 trials of antipsychotic medication of adequate dose and duration.3 Despite its clinical benefits, clozapine has potentially life-threatening side effects, eg, hematologic, metabolic, and cardiac effects.4 Impairment of gastrointestinal motility is also common, with an estimated occurrence of 14%.5 Gastrointestinal hypomotility can lead to paralytic ileus, obstruction, gastrointestinal ischemia, and death.6,7 Herein, a case of clozapine-related cecal volvulus is described. To our knowledge, volvulus associated with clozapine use has only been reported once previously.8 This case illustrates the need for a high index of suspicion for potentially life threatening surgical emergencies in clozapine-treated patients.
Case Report
A 58-year-old woman with schizoaffective disorder, bipolar type, residing in a long-term psychiatric facility for chronically ill patients for 6 years, was transitioned to an acute care hospital for evaluation of constipation, abdominal distention, nausea, and bilious vomiting of 3-day duration. Her psychiatric medications included clozapine 575 mg/d, clonazepam 0.5 mg twice/d as needed, lamotrigine 100 mg/d, and haloperidol 5 mg by mouth 3 times/d as needed. Diphenhydramine 50 mg by mouth 4 times/d as needed was recently initiated for pruritus. She had a history of intermittent constipation but was often nonadherent with a recommended bowel regimen consisting of senna/docusate sodium 8.6/50 twice/d and polyethylene glycol daily. Her bowel habits were not consistently documented. Despite her postmenopausal status and lack of an intimate partner, she attributed the abdominal distention to pregnancy.
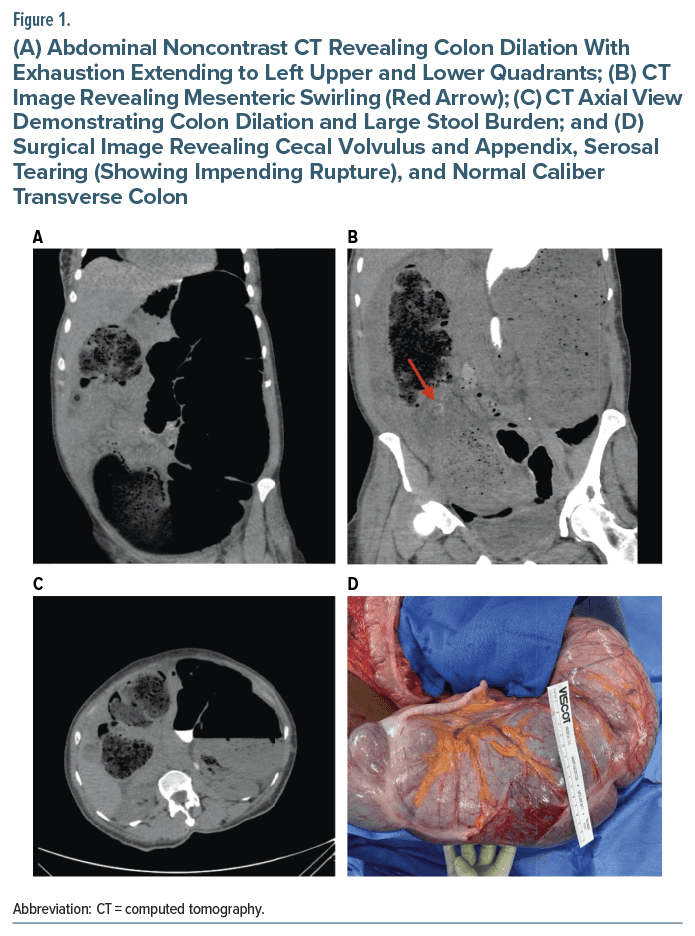
On examination, her vital signs were notable for hypertension, ie, blood pressure of 166/91 mm Hg, but otherwise unremarkable (heart rate: 90 beats/min, respirations: 18/min, and temperature: 36.8°C). The abdomen was distended, soft, and nontender. The comprehensive metabolic panel revealed hypokalemia (2.8 mmol/L) without other significant abnormalities, eg, the lactic acid level was 1.1 mmol/L and complete blood count was unremarkable. Abdominal X-ray revealed marked dilation of the colon containing an air fluid level occupying the left upper and lower quadrants with preservation of haustral folds; air fluid levels were visualized within loops of bowel in the pelvis. Initial clinical impression consisted of Ogilvie syndrome (Figure 1).
Clozapine and diphenhydramine were withheld. The patient was given nothing by mouth, and potassium was repleted; an aggressive bowel regimen including polyethylene glycol, senna, and mineral oil enemas was suggested but thwarted by the patient’s refusal, as she insisted the abdominal distention was from pregnancy. Gastroenterology consultants considered endoscopic decompression but were dissuaded by a significant stool burden that would have prevented access to the right side of the colon. Neostigmine was considered to reverse the anticholinergic influences of the patient’s medication regimen.
Subsequent computed tomography (CT) imaging of the abdomen/pelvis with rectal contrast showed progression of the contrast to the splenic flexure/transverse colon and revealed mesenteric swirling (Figure 1) in the right lower quadrant adjacent to a dilated nonopacified loop of bowel measuring 11 cm and extending to the left hemiabdomen. Cecal volvulus was suspected despite the lack of significant small bowel dilation. Surgical intervention, ie, exploratory laparotomy, confirmed cecal volvulus and tearing of the intestinal serosa, indicating impending rupture (see Figure 1). The transverse colon, descending colon, sigmoid, and rectum appeared healthy. A right hemicolectomy with stapled side-to side anastomosis was performed without complications. Bowel motility was restored; she progressed well postoperatively and returned to the long-term facility.
Discussion
Generally, the anticholinergic, serotonergic, and noradrenergic effects of clozapine are implicated in producing clozapine-induced gastric hypomotility (CIGH).8 CIGH is managed effectively with laxatives, stool softeners, and dietary modifications.7 For clozapine-treated patients developing abdominal pain and distention, vomiting, and marked constipation, a careful workup of serious causes, eg, Ogilvie syndrome or cecal volvulus, is warranted. These conditions require aggressive treatment to reduce potential sequelae, ie, perforation, peritonitis, and death. Because symptoms can overlap, distinguishing between Ogilvie syndrome and cecal volvulus is challenging. Contrast-enhanced CT imaging and, in ambiguous cases, abdominal laparotomy are warranted to distinguish them.9
Cecal volvulus rarely occurs in adults and is related to improper fusion of the cecal mesentery with the retroperitoneum predisposing the cecum to rotation and twisting. It occurs in women predominantly, between 40 and 60 years of age.10 Precipitating factors for cecal volvulus include constipation, ileus, and prior surgery with resultant adhesions. Other than recurrent constipation, nothing in the patient’s history suggested that she had any other aggravating risk factors. In fact, CT imaging of her abdomen 4 years earlier revealed that her cecum was large, anteromedially oriented, and mobile; the latter increased her vulnerability to recurrent constipation particularly while on clozapine. Now, exacerbated by an increased anticholinergic burden (ie, the addition of diphenhydramine) and nonadherence with the bowel regimen, she was particularly vulnerable to developing cecal volvulus.
A low threshold of suspicion for potentially emergent surgical conditions is warranted when patients on clozapine develop vomiting, severe constipation, or abdominal distention/ pain. To mitigate risks, clozapine treated patients, particularly in long term care settings, require diligent nursing documentation of bowel habits, fluid and diet/fiber intake, physical activity, adherence with bowel management, and gastrointestinal symptoms.7,11 Reducing the anticholinergic burden and avoiding serotonergic antagonists will also mitigate hypomotility.
Article Information
Published Online: July 11, 2024. https://doi.org/10.4088/PCC.24cr03729
© 2024 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2024;26(4):24cr03729
Submitted: February 23, 2024; accepted April 15, 2024.
To Cite: Bayless SL, Walker NV, Scott MM, et al. Clozapine related cecal volvulus. Prim Care Companion CNS Disord. 2024;26(4):24cr03729.
Author Affiliation: Department of Psychiatry, University at Buffalo, Jacobs School of Medicine and Biomedical Sciences, Buffalo, New York (all authors).
Corresponding Author: Raphael J. Leo, MD, MA, Department of Psychiatry, University at Buffalo, Jacobs School of Medicine and Biomedical Sciences, Erie County Medical Center, 462 Grider St, Buffalo, NY 14215 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Consent was received from the patient to publish the case report, and information was de identified to protect patient anonymity.
References (11)

- Mortimer AM. Antipsychotic treatment in schizophrenia: atypical options and NICE guidance. Eur Psychiatry. 2003;18(5):209–219. PubMed CrossRef
- Siskind D, McCartney L, Goldschlager R, et al. Clozapine v. first- and second-generation antipsychotics in treatment-refractory schizophrenia: systematic review and meta-analysis. Br J Psychiatry. 2016;209(5):385–392. PubMed CrossRef
- Howes OD, McCutcheon R, Agid O, et al. Treatment resistant schizophrenia: treatment response and resistance in psychosis (TRRIP) working group consensus guidelines on diagnosis and terminology. Am J Psychiatry. 2017;174(3):216–229. PubMed CrossRef
- De Berardis D, Rapini G, Olivieri L, et al. Safety of antipsychotics for the treatment of schizophrenia: a focus on the adverse effects of clozapine. Ther Adv Drug Saf. 2018;9(5):237–256. PubMed CrossRef
- Novartis Pharmaceuticals Canada Inc. Clozaril Product Monograph. Revised. 2004.
- Every-Palmer S, Inns SJ, Grant E, et al. Effects of clozapine on the gut: cross-sectional study of delayed gastric emptying and small and large intestinal dysmotility. CNS Drugs. 2019;33(1):81–91. PubMed
- Hibbard KR, Propst A, Frank DE, et al. Fatalities associated with clozapine-related constipation and bowel obstruction: a literature review and two case reports. Psychosomatics. 2009;50(4):416–419. PubMed CrossRef
- Aneja J, Varshney V, Ks S, et al. Clozapine triggering cecal volvulus in a patient with malrotation and schizophrenia: side effect that needs emphasis. Cureus. 2020;12(5):e7971. PubMed CrossRef
- Tampakis A, Droeser RA, Tampaki EC, et al. A case of cecal volvulus mimicking Ogilvie syndrome in a hospitalized patient with a pelvis fracture. Ann Med Surg (Lond). 2016;7:55–57. PubMed CrossRef
- Atamanalp SS, Ozogul B, Kisaoglu A. Cecal volvulus: a rare cause of intestinal obstruction. Eurasian J Med. 2012;44(2):115–116. PubMed CrossRef
- Hayes G, Gibler B. Clozapine-induced constipation. Am J Psychiatry. 1995;152(2):298. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!