Anorexia nervosa (AN) is the second most lethal psychiatric disorder behind substance use disorders.1 Patients with comorbid AN and alcohol use disorder (AUD) have 10 times the risk of mortality compared to patients without AUD.1 Patients with AN have an increased risk of developing AUD2: 1 in 5 patients with any eating disorder will abuse alcohol in their lifetime.3 In this report, we highlight associations between AN and AUD, emphasizing biological and psychological aspects of both conditions.
Case Report
Ms D is a 57-year-old woman with a medical history of osteoporosis, headaches, gastroesophageal reflux disease, irritable bowel syndrome, major depressive disorder, AN, anxiety, and AUD. She was referred from neurology for outpatient psychiatric consultation given her complex psychiatric history.
Ms D describes disordered eating behaviors including food avoidance and restriction, with compensatory behaviors such as self-induced vomiting; use of laxatives, diuretics, and enemas; and extreme exercise. Her eating problems stem from early childhood experiences revolving around control and sibling rivalry. Although her current body mass index is 15 kg/m2, she continued to weigh herself daily, believing she was overweight. She also reports neurovegetative symptoms of depression, comorbid anxiety, and history of abuse but denies trauma related symptoms. Ms D began using alcohol in college but then transitioned to daily alcohol use in her 40s. She continues to use alcohol on a daily basis to stimulate her appetite.
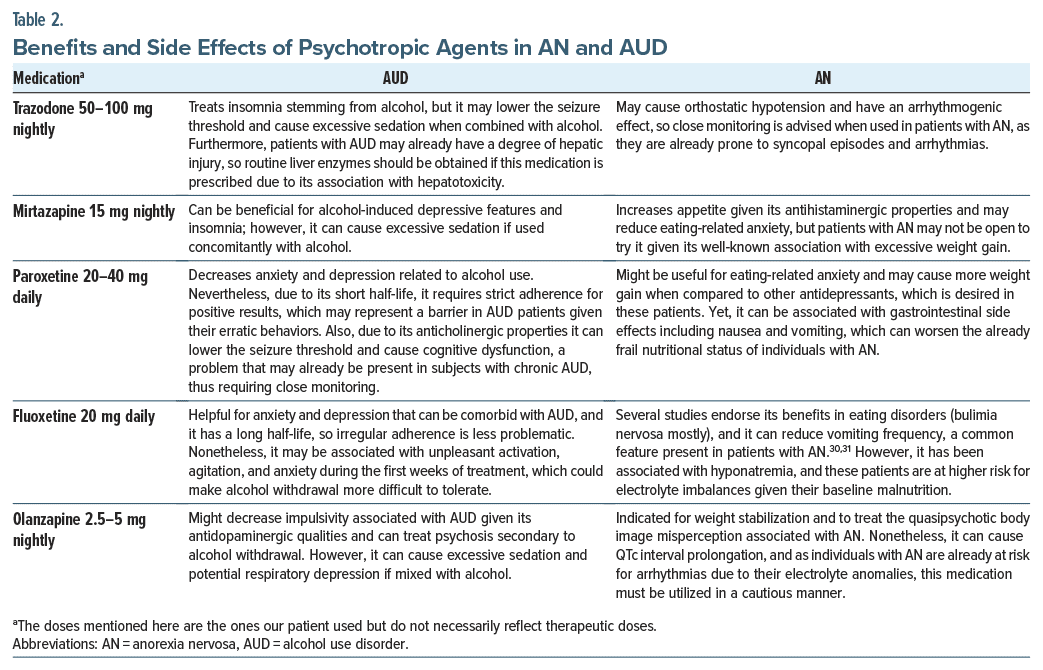
Complete blood count, comprehensive metabolic panel, thyroid function tests, vitamin levels, and estradiol parameters are all within normal range, but her lipase level is increased. Recent brain magnetic resonance imaging with and without contrast revealed evidence of a remote ischemic event in the frontal area with no acute anomalies, and cortical volume is age appropriate. The psychiatry team recommended that Ms D transition from paroxetine to fluoxetine and initiate olanzapine to target insomnia, poor appetite, impulsivity, and depression. She declined medications for AUD or referrals to eating disorder programs.
After a subsequent follow-up with her primary care provider, olanzapine was initiated, and she was advised to decrease her alcohol intake. She declined to start fluoxetine, fearing side effects and hepatotoxicity, instead opting to continue paroxetine. She initially reported benefit from olanzapine, though subsequently self-discontinued it after reporting insomnia and palpitations. She ultimately elected to transfer care to her local community mental health center to access more comprehensive psychiatric care.
Discussion
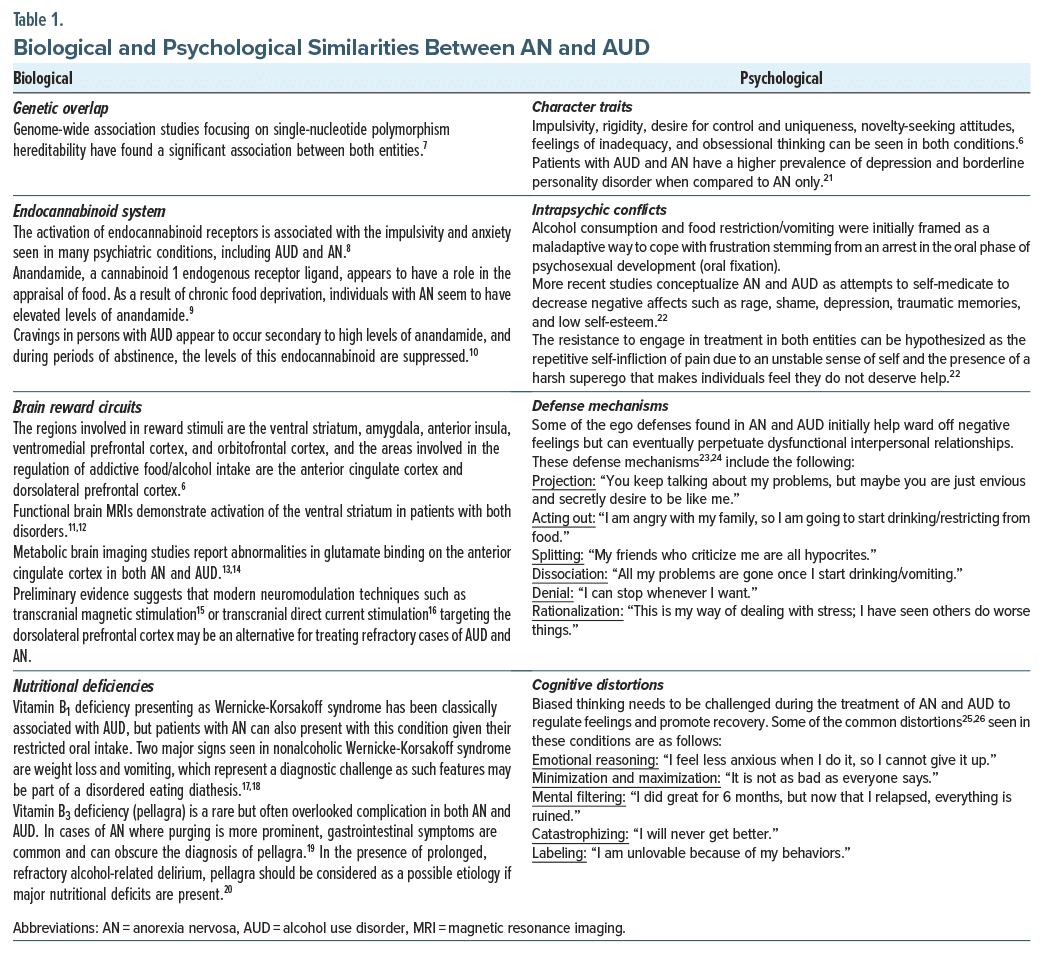
AN and AUD share several biological and psychological features. As an example, both entities can exhibit cardiac dysfunction.4,5 Likewise, given their underlying deficits in oral intake, patients with AN and AUD are prone to hypokalemia and hypomagnesemia, which can lead to QTc prolongation and subsequent limitations in the use of psychotropic agents.6 Other biopsychological characteristics seen in both disorders are described in Table 1. These include genetic aspects,7 alterations in the endocannabinoid8–10 and brain reward systems,6,11–16 nutritional deficiencies,17–20 character traits,6,21 intrapsychic conflicts,22 defense mechanisms,23,24 and cognitive distortions.25,26 A clear illustration of the psychological complexities seen in both AUD and AN was the degree of cognitive dissonance present in this patient: she considered herself to be overweight, but she also used alcohol to stimulate her appetite—the natural outcome of an increase in appetite is weight gain, which was also her biggest fear. Noteworthy, as subjects with AN and AUD suffer from complex medical comorbidities,4,5,19,20 routine monitoring of side effects is advised when prescribing psychotropic agents. The patient described here tried different antidepressants and antipsychotics for her symptoms, including medications that had been utilized years before our initial encounter with her. The advantages and disadvantages27–31 of these specific agents when treating individuals with AN and AUD are delineated in Table 2.
Conclusion
AN and AUD share similar etiologic factors. Exploration of biologic, psychodynamic, and cognitive behavioral aspects in AN and AUD is key for treatment purposes. Comorbid AN and AUD carry a poor prognosis, and pertinent screenings should be in place when providing care to these populations.32 Patients with comorbid AN and AUD may benefit from a multimodal treatment approach involving pharmacotherapy and psychotherapy. When feasible, both entities should be treated concurrently. Several interventions have evidence for both AN and AUD such as self-help approaches, cognitive-behavioral therapy, psychodynamic psychotherapy, dialectical behavior therapy, family and couples therapy, and motivational interviewing.32 Psychiatrists, especially those working in embedded/collaborative care settings, can assist with diagnosing and treating these comorbid conditions. Treatments for both AN and AUD are individualized and must take into consideration each patient’s intrinsic motivation and readiness for change.
Article Information
Published Online: November 14, 2024. https://doi.org/10.4088/PCC.24cr03806
© 2024 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2024;26(6):24cr03806
Submitted: July 3, 2024; accepted August 29, 2024.
To Cite: Chen K, Ho P, Calagua-Bedoya EA. The comorbidity between eating disorders and alcohol misuse: biological and psychological perspectives illustrated by a case report. Prim Care Companion CNS Disord. 2024;26(6):24cr03806.
Author Affiliations: Department of Psychiatry, Dartmouth Hitchcock Medical Center, Lebanon, New Hampshire (all authors).
Corresponding Author: Eduardo Andres Calagua-Bedoya, MD, Department of Psychiatry, Dartmouth Hitchcock Medical Center, One Medical Center Drive, Lebanon, NH 03756 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Previous Presentation: Poster presented at the 2024 APA Annual Meeting; May 4–8, 2024; New York, New York.
Patient Consent: Consent was received from the patient to publish the case report, and information has been de identified to protect patient anonymity.
References (32)

- Mellentin AI, Mejldal A, Guala MM, et al. The impact of alcohol and other substance use disorders on mortality in patients with eating disorders: a nationwide register-based retrospective cohort study. Am J Psychiatry. 2022;179(1):46–57. PubMed
- Mellentin AI, Skøt L, Guala MM, et al. Does receiving an eating disorder diagnosis increase the risk of a subsequent alcohol use disorder? A Danish nationwide register-based cohort study. Addiction. 2022;117(2):354–367. PubMed CrossRef
- Bahji A, Mazhar MN, Hudson CC, et al. Prevalence of substance use disorder comorbidity among individuals with eating disorders: a systematic review and meta-analysis. Psychiatry Res. 2019;273:58–66. PubMed CrossRef
- Cost J, Krantz MJ, Mehler PS. Medical complications of anorexia nervosa. Cleve Clin J Med. 2020;87(6):361–366. PubMed CrossRef
- Rehm J, Hasan OSM, Imtiaz S, et al. Quantifying the contribution of alcohol to cardiomyopathy: a systematic review. Alcohol. 2017;61:9–15. PubMed CrossRef
- Devoe DJ, Dimitropoulos G, Anderson A, et al. The prevalence of substance use disorders and substance use in anorexia nervosa: a systematic review and meta-analysis. J Eat Disord. 2021;9(1):161. PubMed CrossRef
- Munn-Chernoff MA, Johnson EC, Chou YL, et al. Shared genetic risk between eating disorder- and substance use-related phenotypes: evidence from genome-wide association studies. Addict Biol. 2021;26(1):e12880. PubMed CrossRef
- Moreira FA, Jupp B, Belin D, et al. Endocannabinoids and striatal function: implications for addiction-related behaviours. Behav Pharmacol. 2015;26(1–2):59–72. PubMed CrossRef
- Monteleone P, Maj M. Dysfunctions of leptin, ghrelin, BDNF and endocannabinoids in eating disorders: beyond the homeostatic control of food intake. Psychoneuroendocrinology. 2013;38(3):312–330. PubMed CrossRef
- Mangieri RA, Hong KIA, Piomelli D, et al. An endocannabinoid signal associated with desire for alcohol is suppressed in recently abstinent alcoholics. Psychopharmacology (Berl). 2009;205(1):63–72. PubMed CrossRef
- Fladung AK, Schulze UME, Schöll F, et al. Role of the ventral striatum in developing anorexia nervosa. Transl Psychiatry. 2013;3(10):e315. PubMed CrossRef
- Schacht JP, Anton RF, Myrick H. Functional neuroimaging studies of alcohol cue reactivity: a quantitative meta-analysis and systematic review. Addict Biol. 2013;18(1):121–133. PubMed CrossRef
- Godlewska BR, Pike A, Sharpley AL, et al. Brain glutamate in anorexia nervosa: a magnetic resonance spectroscopy case control study at 7 Tesla. Psychopharmacology (Berl). 2017;234(3):421–426. PubMed CrossRef
- Akkus F, Mihov Y, Treyer V, et al. Metabotropic glutamate receptor 5 binding in male patients with alcohol use disorder. Transl Psychiatry. 2018;8(1):17. PubMed CrossRef
- Sorkhou M, Stogios N, Sayrafizadeh N, et al. Non invasive neuromodulation of dorsolateral prefrontal cortex to reduce craving in alcohol use disorder: a meta analysis. Drug Alcohol Depend Rep. 2022;4:100076. PubMed CrossRef
- Chmiel J, Gladka A, Leszek J. The effect of transcranial direct current stimulation (tDCS) on anorexia nervosa: a narrative review. Nutrients. 2023;15(20):4455. PubMed CrossRef
- Ho PA, York A, Rustad JK, et al. Non-alcohol-related Wernicke’s encephalopathy: diagnosis and treatment. Prim Care Companion CNS Disord. 2021;23(5):21f02968. PubMed CrossRef
- Oudman E, Wijnia JW, Oey MJ, et al. Wernicke-Korsakoff syndrome despite no alcohol abuse: a summary of systematic reports. J Neurol Sci. 2021;426:117482. PubMed CrossRef
- Onteeru M. Pellagra as a potential complication of anorexia nervosa: a comprehensive literature review. Hum Nutr Metabolism. 2023;32:200197.
- Oldham MA, Ivkovic A. Pellagrous encephalopathy presenting as alcohol withdrawal delirium: a case series and literature review. Addict Sci Clin Pract. 2012;7(1):12. PubMed CrossRef
- Baker JH, Thornton LM, Strober M, et al. Temporal sequence of comorbid alcohol use disorder and anorexia nervosa. Addict Behav. 2013;38(3):1704–1709. PubMed CrossRef
- Gabbard GO. Psychodynamic Psychiatry in Clinical Practice. 5th ed. American Psychiatric Publishing, Inc; 2014.
- Gothelf D, Apter A, Ratzoni G, et al. Defense mechanisms in severe adolescent anorexia nervosa. J Am Acad Child Adolesc Psychiatry. 1995;34(12):1648–1654. PubMed CrossRef
- Taurino A, Antonucci LA, Taurisano P, et al. Investigating defensive functioning and alexithymia in substance use disorder patients. BMC Psychiatry. 2021;21(1):337. PubMed
- Ruiz Santos P, Barey AF, Pautassi RM. Cognitive distortions associated with alcohol and marijuana use in Uruguayan citizens. Subst Use Misuse. 2024;59(5):680–689. PubMed
- Costin C, Grabb GS, Rothschild B. 8 Keys to Recovery From an Eating Disorder: Effective Strategies From Therapeutic Practice and Personal Experience (8 Keys to Mental Health). W. W. Norton; 2011.
- Stahl SM. Stahl’s Essential Psychopharmacology: Prescriber’s Guide. Cambridge University Press; 2024.
- Gill H, Gill B, El-Halabi S, et al. Antidepressant medications and weight change: a narrative review. Obes (Silver Spring). 2020;28(11):2064–2072.
- Todorović Vukotić N, Dordević J, Pejić S, et al. Antidepressants- and antipsychotics-induced hepatotoxicity. Arch Toxicol. 2021;95(3):767–789. PubMed
- Muratore AF, Attia E. Psychopharmacologic management of eating disorders. Curr Psychiatry Rep. 2022;24(7):345–351. PubMed CrossRef
- Frank GKW. Pharmacotherapeutic strategies for the treatment of anorexia nervosa: too much for one drug? Expert Opin Pharmacother. 2020;21(9):1045–1058. PubMed CrossRef
- Gregorowski C, Seedat S, Jordaan GP. A clinical approach to the assessment and management of comorbid eating disorders and substance use disorders. BMC Psychiatry. 2013;13:289. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!