Delusions of parasitosis (DP), also known as delusional infestation, psychogenic parasitosis, formication, or Ekbom syndrome, is characterized by abnormal cutaneous sensations with no objective evidence to support an underlying dermatologic condition. An elderly patient developed DP with extended-release methylphenidate (MPH) after taking it for more than 6 years. DP resolved when it was discontinued and did not reoccur after switching to an equivalent dose of dextroamphetamine/amphetamine. Although psychosis is a well-known complication of stimulants, amphetamines are associated with a greater risk of psychosis compared to MPH formulations. This case contributes to the literature by demonstrating that the patient’s psychosis was triggered by MPH but did not reoccur after nearly 2.5 years on an equivalent dose of mixed amphetamine salts, followed by a slightly higher dose for the past 2 months (to date).
Case Report
A 70-year-old woman with a history of recurrent depression, generalized anxiety disorder, and attention-deficit/hyperactivity disorder (ADHD) was treated with MPH extended-release 36 mg, aripiprazole 5 mg, gabapentin 900 mg, and trazodone 100–200 mg daily. She had discontinued sertraline due to its potential adverse impact on her dental implants and preferred to continue with aripiprazole, which had been added to sertraline for treating depression. Her history was negative for psychosis, hospitalizations, and stimulant or substance abuse. Past medications included lisdexamfetamine 70 mg daily, amphetamine salts 20–40 mg, atomoxetine, and sertraline.
The patient reported experiencing painful, nonitchy “insect bites” on her back and other parts of her body, accompanied by visual hallucinations of bugs in her house and clothing for over 2.5 years. She emailed pictures of her scalp and sputum, claiming to see worms (Figs. 1 and 2). She brought multiple plastic bags containing inanimate objects (hair/paper-like debris) and reported having over 300 photographs of the insects. She saw flea-like insects, bugs with feathers, a “black thread-like object” emerging from her skin, and blood with a dead bug while cleaning her ears.
On examination, the patient had sporadic erythematous macules on her upper back. Head computed tomography, thyroid-stimulating hormone levels, and vitamin B1, B12, D, and B6 levels were all within normal limits. No underlying medical condition, including syphilis, was identified, and multiple urine drug screens were negative.
She was resistant to reducing or stopping MPH, so aripiprazole was gradually increased to 20 mg daily, but it provided no benefit. Her symptoms eventually resolved completely after discontinuing MPH. Later, trials of guanfacine, atomoxetine, and lisdexamfetamine were unsatisfactory. Subsequently, dextroamphetamine/amphetamine was initiated and gradually increased to 20 mg daily. This was therapeutic with no reoccurrence of psychosis when taken for almost 2.5 years. The dose of dextroamphetamine/ amphetamine was increased 2 months ago, at the time of this writing, from 20 mg to 30 mg and was tolerated well.
Discussion
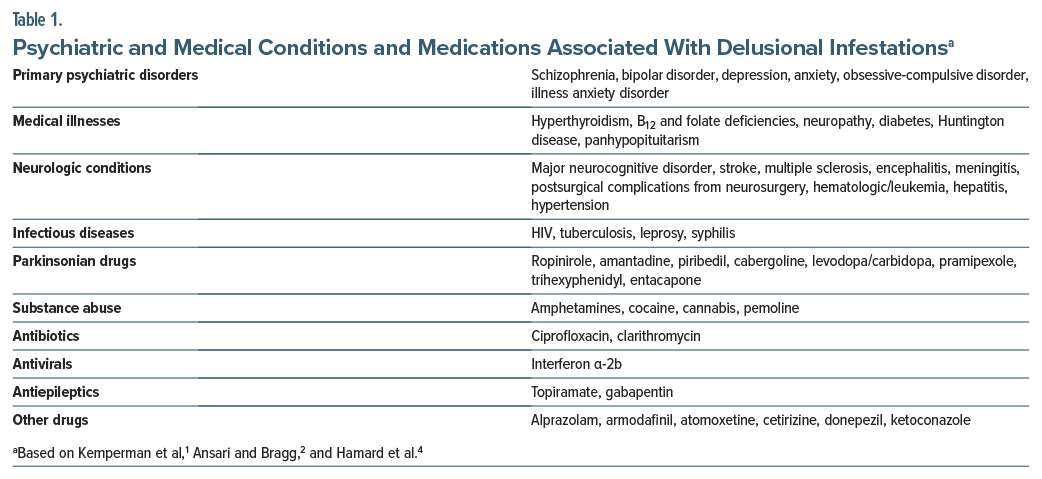
Psychogenic parasitosis, first described about a century ago, can occur secondary to various psychiatric and medical conditions, substance abuse, or as an adverse reaction to several classes of medications (Table 1).1,2 The “matchbox sign” is a classic presentation in which patients bring “parasites” they believe are infesting them. Complex visual hallucinations, as seen in this patient, have been reported with MPH.3 Psychostimulants increase dopaminergic and noradrenergic neurotransmission, leading to dysregulation of the striatal dopamine system. Long-term use of MPH can reduce brain dopamine transporter density in the striatum, causing excessive synaptic dopamine.3 Additionally, hyperactivity of serotonin receptors may play a role in psychosis onset.1
Several studies found no increase in psychosis risk with MPH compared to placebo.5–7 A large cohort study8 of 221,000 adolescents and young adults with ADHD found that amphetamines were associated with double the risk of psychosis compared to MPH formulations.
Recent studies also concluded that amphetamines were associated with a higher occurrence of psychosis compared with MPH use.4,9 A dose responsive relationship was noted, and doses higher than 30 mg of dextroamphetamine were associated with 5.28-fold increased odds of psychosis or mania.9 Studies have also shown that the release of dopamine may be 4 times greater with amphetamine compared to MPH.10
However, in the present case, MPH precipitated psychosis, while amphetamine salts were better tolerated. The patient took stimulants for decades and had been on MPH for over 6 years before developing DP.
Further research is needed to better understand the pharmacologic mechanisms underlying stimulant induced DP. Advanced functional brain imaging may help identify the areas of the brain involved, as well as other pathways, apart from those related to ADHD. A study reviewing 60 cases of stimulant-induced psychotic or manic symptoms found that these symptoms resolved after dose reduction or discontinuation of stimulant in 92% of cases. In the remaining 8%, ongoing psychosis led to a rediagnosis of either bipolar disorder or schizophrenia.11 The current patient’s symptoms resolved only after discontinuing MPH and did not recur during nearly 2.5 years of taking 20 mg of mixed amphetamine salts daily, followed by 30 mg daily for the next 2 months. Given the potential vulnerability of elderly patients, stimulant use should be approached with caution.
Article Information
Published Online: April 29, 2025. https://doi.org/10.4088/PCC.24cr03880
© 2025 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2025;27(2):24cr03880
Submitted: October 27, 2024; accepted January 14, 2025.
To Cite: Hafeez ZH. Delusions of parasitosis with extended-release methylphenidate in an elderly woman. Prim Care Companion CNS Disord 2025;27(2):24cr03880.
Author Affiliation: Kaiser Permanente Santa Rosa, Santa Rosa, California (Hafeez).
Corresponding Author: Zeba Hasan Hafeez, MD, Kaiser Permanente Santa Rosa, 3554 Roundbarn Blvd, Santa Rosa, CA 95403 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Consent was received from the patient to publish the case report and photos, and information has been de-identified to protect anonymity.
References (11)

- Kemperman PMJH, Bruijn TVM, Vulink NCC, et al. Drug-induced delusional infestation. Acta Derm Venereol. 2022;102:adv00663. CrossRef
- Ansari MN, Bragg BN. Delusions of parasitosis. In: Stat Pearls [Internet]. StatPearls Publishing; 2023.
- Halevy A, Shuper A. Methylphenidate induction of complex visual hallucinations. J Child Neurol. 2009;24(8):1005–1007. CrossRef
- Hamard J, Rousseau V, Durrieu G, et al. Psychosis with use of amphetamine drugs, methylphenidate and atomoxetine in adolescent and adults. BMJ Ment Health. 2024;27:e300876–e300877. CrossRef
- Hollis C, Chen Qi, Chang Z, et al. Methylphenidate and the risk of psychosis in adolescents and young adults: a population-based cohort study. Lancet Psychiatry. 2019;6(8):651–658. CrossRef
- Gallagher KE, Melissa C, Funaro MC, et al. Prescription stimulants and the risk of psychosis: a systematic review of observational studies. J Clin Psychopharmacol. 2022;42(3):308–314.
- Man KKC, Coghill D, Chan EW, et al. Methylphenidate and the risk of psychotic disorders and hallucinations in children and adolescents in a large health system. Transl Psychiatry. 2016;6(11):e956. CrossRef
- Moran LV, Ongur D, Hsu J, et al. Psychosis with methylphenidate or amphetamine in patients with ADHD. N Engl J Med. 2019;380(12):1128–1138. CrossRef
- Moran LV, Skinner JP, Shinn AK, et al. Risk of incident psychosis and mania with prescription amphetamines. Am J Psychiatry. 2024;181(10):901–909. CrossRef
- Schiffer WK, Volkow ND, Fowler JS, et al. Therapeutic doses of amphetamine or methylphenidate differentially increase synaptic and extracellular dopamine. Synapse. 2006;59(4):243–251. CrossRef
- Slaughter JR, Zanol K, Rezvani H, et al. Psychogenic parasitosis. A case series and literature review. Psychosomatics. 1998;39(6):491–500. CrossRef
Enjoy this premium PDF as part of your membership benefits!