Factitious disorder, characterized by the intentional production or exaggeration of symptoms for the primary purpose of assuming the sick role, was first defined as Munchausen syndrome by Asher in 1951.1,2 Unlike malingering, which is driven by external gains, factitious disorder is motivated by internal psychological needs.3 This condition presents significant diagnostic challenges, particularly in adolescents, in whom differentiating genuine from fabricated symptoms is complex.4 Factitious disorder is estimated to occur in 0.5%–2% of internal medicine settings, but reliable statistics for the broader US population are lacking.4
The case discussed here is notable for the frequent hospital admissions of an adolescent patient and the eventual discovery that his symptoms were self induced to escape an abusive home environment. This case underscores the importance of comprehensive assessments, including psychosocial evaluations, and highlights the need to consider underlying psychological conditions in adolescent patients presenting with recurrent unexplained medical symptoms.
Case Report
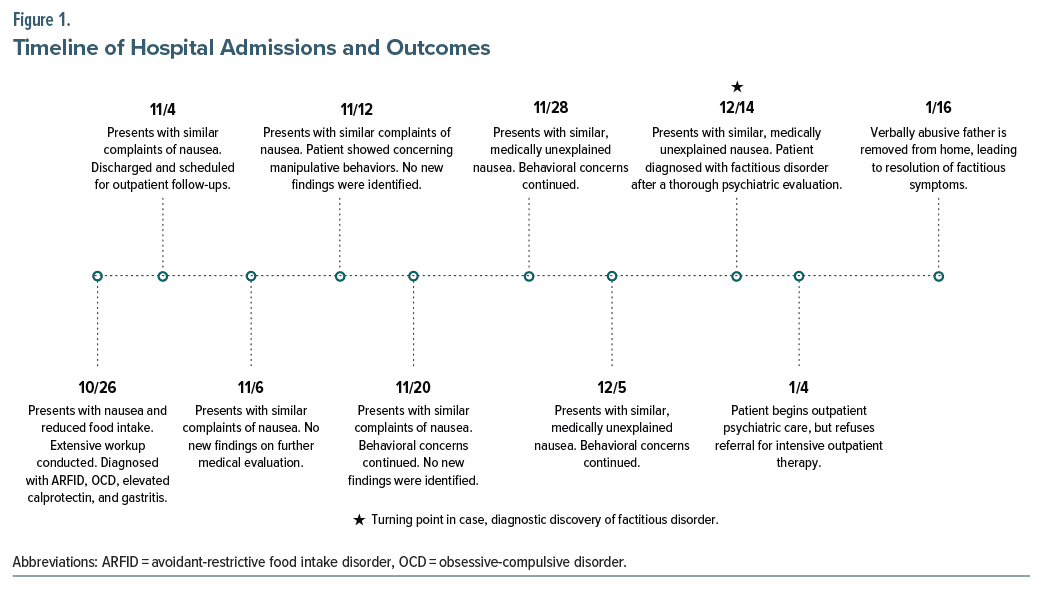
A 14-year-old boy with no prior psychiatric history was admitted to the hospital 8 times over 3 months (October 26th, November 4th, November 6th, November 12th, November 20th, November 28th, December 5th, and December 14th) for intractable nausea and reduced food intake. Initial diagnoses included avoidant-restrictive food intake disorder (ARFID), obsessive compulsive disorder, elevated calprotectin, and gastritis. Despite appropriate medical and psychiatric interventions, the patient continued to exhibit symptoms and declined outpatient care in favor of readmission.
During hospital stays, manipulative behaviors such as tampering with medical equipment and making unnecessary medical requests were observed. A comprehensive psychiatric evaluation during his eighth admission revealed significant family stress, including verbal abuse at home. The patient ultimately admitted to fabricating symptoms to prolong his hospital stays, which he viewed as a refuge from his challenging home environment.
Approximately 1 month after discharge, the patient’s father moved out of the home, leading to an immediate and complete resolution of the factitious symptoms. Since then, the patient has maintained good health and reports no recurrence of previous symptoms. He now has limited contact with his father, reducing his exposure to the verbal stressors that had initially contributed to the development of his symptoms.
Treatment included medication management for anxiety (fluoxetine and propranolol) and referrals for outpatient therapy. Despite recommendations for intensive outpatient therapy, the patient’s mother preferred managing his care at home. A child protective services report was filed to assess the home environment, and the patient began attending an outpatient psychiatric clinic but declined therapy. Figure 1 describes the patient’s hospital admissions and outcomes.
Discussion
This case illustrates the complexities of diagnosing factitious disorder in adolescents, wherein psychosocial factors play a significant role. The patient’s intentional production of symptoms to escape abuse highlights the critical need for thorough psychosocial evaluations in cases of recurrent unexplained symptoms.5 The diagnostic process was challenging, with differential diagnoses initially considered, including ARFID and chronic gastrointestinal conditions. The pattern of hospital admissions, lack of consistent medical findings, and the patient’s admission of symptom fabrication ultimately led to the factitious disorder diagnosis.
The resolution of symptoms following his father’s departure provides additional support for the diagnosis. The removal of stressors associated with the patient’s verbally abusive home environment aligns with DSM-5 criteria for factitious disorder and reinforces the impact of environmental changes on symptom resolution.6 While previous hospitalizations may have been partially a cry for help, the complete cessation of symptom falsification in the absence of stressors further confirms the diagnosis. This case demonstrates that removing environmental stressors can be instrumental in symptom resolution, highlighting the need for holistic care in adolescent psychiatric cases where factitious disorder is suspected.
The case underscores the importance of a multidisciplinary approach involving medical, psychiatric, and social work professionals. Screening tools and comprehensive psychiatric evaluations are essential in identifying underlying issues. Therapists play a crucial role in addressing maladaptive coping strategies, while social workers are vital in assessing and intervening in the patient’s home environment.
Conclusion
This case highlights the need for a comprehensive approach to adolescents with recurrent, unexplained symptoms. Given the link between child maltreatment, including verbal abuse, and mental health disorders, it is vital to consider these social factors. Integrating medical and psychological evaluations can reveal underlying issues like factitious disorder, emphasizing holistic care. The interdisciplinary management of this patient demonstrates the importance of collaboration between medical and mental health professionals in complex cases. This case enhances our understanding of factitious disorder in adolescents and underscores the role of family dynamics in presenting symptoms, advocating for more integrated care strategies in the future.
Article Information
Published Online: February 27, 2025. https://doi.org/10.4088/PCC.24cr03832
© 2025 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2025;27(1):24cr03832
Submitted: August 15, 2024; accepted December 2, 2024.
To Cite: McDuffee NS, Forster AA, Shah K, et al. Factitious disorder in the context of abuse in an adolescent: importance of a multidisciplinary approach. Prim Care Companion CNS Disord. 2025;27(1):24cr03832.
Author Affiliations: Wake Forest School of Medicine, Winston-Salem, North Carolina (McDuffee, Forster); Atrium Health Wake Forest Baptist, Winston-Salem, North Carolina (Shah, Easterday)
Corresponding Author: Nicholas S. McDuffee, MA, BS, Department of Psychiatry, Wake Forest School of Medicine, Atrium Health Wake Forest Baptist, 1 Medical Center Blvd, Winston-Salem, North Carolina, 27157 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Consent was received from the patient to publish the case report, and information, including dates, has been de-identified to protect anonymity.
References (6)

- Asher R. Munchausen’s syndrome. Lancet. 1951;1:339–341.
- Yates GP, Feldman MD. Factitious disorder: a systematic review of 455 cases in the professional literature. Gen Hosp Psychiatry. 2016;41:20–28. PubMed CrossRef
- Bass C, Wade DT. Malingering and factitious disorder. Pract Neurol. 2019;19(2):96–105. PubMed CrossRef
- Jaghab K, Skodnek KB, Padder TA. Munchausen’s syndrome and other factitious disorders in children: case series and literature review. Psychiatry. 2006;3(3):46–55. PubMed
- Mathews B, Pacella R, Dunne M, et al. The Australian Child Maltreatment Study (ACMS): protocol for a national survey of the prevalence of child abuse and neglect, associated mental disorders and physical health problems, and burden of disease. BMJ Open. 2021;11(5):e047074. PubMed
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
Enjoy this premium PDF as part of your membership benefits!