The frontal lobe represents over a third of the human brain and is associated with complex cognitive functions and behaviors characteristic of adulthood. Prefrontal syndromes result from damage to the prefrontal lobes and can be categorized into 3 types based on specific frontal-subcortical circuits affected: the medial frontal circuit (causing apathy, abulia, and akinetic mutism), the dorsolateral prefrontal circuit (impairing executive functions), and the orbitofrontal circuit (leading to personality disturbances, affective issues, and social conduct problems).1
Case Report
A 55-year-old man was admitted to the psychiatric emergency department with a warrant due to changes in behavior, posing risk to himself and to others, and refusing medical assistance. Family and coworkers reported that over the past 7 years his behavior had changed: he became distrustful and less friendly at work, was frequently in conflict with coworkers, and suspected his neighbors were interested in his wife and that she was involved with them. He displayed hypersexual and coercive behavior toward his wife, who accused him of domestic violence, as he tried to control her and exhibited aggressive behavior, preventing her from having a professional life and relationships. Additionally, he had disrupted sleep, started running 2.5 hours daily, and lost 20 kg (44 lb) in 2 years despite eating large amounts of food with increased appetite. Over the past year, he became more irritable, with frequent clastic crisis, and his wife noted increased falls and involuntary movements of the head.
He had no relevant medical history, although his father died in his 50s after becoming ill and was described as “crazy” in his last years. However, it was not possible to clarify his family history.
During observation, mild involuntary choreiform movements of the head and trunk were noted, along with motor impersistence in tongue protrusion and impaired heel-toe walking. He displayed a suspicious posture and evasive speech, along with jealous delusional ideas, irritable mood, and compulsive behaviors (overexercising, hyperphagia, and hypersexuality). Notable weight loss and a disrupted sleep pattern were also observed. He had no insight for the symptoms or need of treatment.
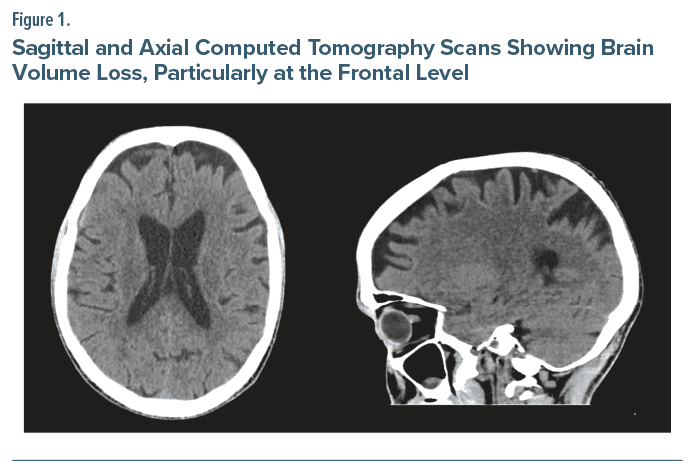
Considering the frontal lobe syndrome presented, a brief neuropsychological evaluation detected deficits in executive function. To investigate the cause of this syndrome, complete blood tests; thoracic, abdominal, and pelvic computed tomography (CT) scan; and electroencephalogram were done and showed no abnormalities. A brain CT scan revealed a moderate pattern of brain volume loss with accentuation of extraventricular cerebrospinal fluid spaces, especially at the frontal level (Figure 1). A frontotemporal dementia was hypothesized, but considering the motor syndrome and the possibility of a movement disorder like Huntington’s disease, genetic testing was conducted and confirmed this diagnosis (42 cytosine, adenine, guanine repeats in the Huntingtin gene).
Discussion
Huntington’s disease is an autosomal dominant genetic disorder that manifests as a progressive neurodegenerative condition. It typically begins in midlife and is characterized by motor, cognitive, and psychiatric symptoms. While motor symptoms are the most distinctive feature, psychiatric symptoms often appear decades earlier and, along with weight loss and sleep disturbances, are common in about half of all Huntington’s disease patients. Psychiatric symptoms include irritability, apathy, anosognosia, depression, sleep disturbances, obsessive and compulsive symptoms, psychosis, suicidal ideation, disinhibition, impulsivity, and dysexecutive behaviors.2,3
Clinicians should be aware of the high rate of psychiatric symptoms in Huntington’s disease, as they often manifest before motor symptoms, causing significant functional impairment.4 These symptoms should be addressed to permit earlier diagnosis and intervention, improving prognosis and providing better sociofamily support and quality of life for patients and their families. This case highlights that frontal lobe syndrome should prompt consideration of Huntington’s disease as a differential diagnosis, even in the absence of typical motor symptoms.2
Article Information
Published Online: February 20, 2025. https://doi.org/10.4088/PCC.24cr03827
© 2025 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2025;27(1):24cr03827
Submitted: August 6, 2024; accepted November 11, 2024.
To Cite: Silva AF, Lopes RM, Fernandes IS. Frontal lobe syndrome unveils an unexpected diagnosis. Prim Care Companion CNS Disord. 2025;27(1):24cr03827.
Author Affiliations: Department of Psychiatry and Mental Health of Unidade Local de Saúde do Médio Tejo, Tomar, Portugal (all authors).
Corresponding Author: André Ferreira Silva, MD, Unidade Local de Saúde do Médio Tejo, Hospital Nossa Senhora da Graça, Av. Maria de Lourdes de Mello e Castro, Tomar 2300-625, Portugal ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Consent was received from the patient to publish the case report, and information has been de identified to protect anonymity.
Acknowledgment: The authors thank Ana Massano, MD, neurologist at Unidade Local de Saúde do Médio Tejo, for providing feedback on the diagnosis of the patient. Dr Massano has no conflicts of interest related to the report.
ORCID: André Ferreira Silva: https://orcid.org/0000-0003-3212-2419; Inês Silva Fernandes: https://orcid.org/0000-0003-4262-3145; Rita Machado Lopes: https://orcid.org/0009-0006-9677-6541
References (4)

- Catani M. The anatomy of the human frontal lobe. In: The Frontal Lobes. 1st ed. Elsevier;2019:95–122. CrossRef
- Goh AMY, Wibawa P, Loi SM, et al. Huntington’s disease: neuropsychiatric manifestations of Huntington’s disease. Australas Psychiatry. 2018;26(4):366–375. PubMed CrossRef
- Karagas NE, Rocha NP, Stimming EF. Irritability in Huntington’s disease. J Huntington’s Dis. 2020;9(2):107–113. PubMed CrossRef
- Sellers J, Ridner SH, Claassen DO. A systematic review of neuropsychiatric symptoms and functional capacity in Huntington’s disease. J Neuropsychiatry Clin Neurosci. 2020;32(2):109–124. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!