Marijuana is a substance derived from the cannabis plant, the active ingredient of which is delta-9 tetrahydrocannabinol, that exhibits its effects within a very short time. Marijuana is mostly inhaled via joints, pipes, bongs, or other methods. A correlation exists between substance use and neuropsychiatric complications such as various cerebrovascular diseases, multifocal leukoencephalopathy, sensory deficits, and movement disorders. Patients were reported to develop toxic leukoencephalopathy after heroin, cocaine, and methamphetamine exposure in the literature.1–3 However, our literature review revealed no cases of toxic leukoencephalopathy associated with cannabis use. We report the case of a male patient with diffused signal and spongiform changes in the brain due to cannabis use. The case was developed based on CARE guidelines.4
Case Report
A 27-year-old single man with a high school education presented to the emergency department (ED) with dysarthric speech, blurred vision, intense tingling sensation, numbness in the hands and feet, and weakness complaints that had persisted intermittently for about 10 days. He was admitted to the neurology clinic with a preliminary diagnosis of demyelinating disease. His relatives revealed that the patient experienced similar symptoms about 7 to 8 years ago for which he presented to the ED and received outpatient treatment; however, no imaging procedure was performed. The patient stated that he intensively used cannabis almost every day, often via inhalation from a bong. The anamnesis presented by the patient revealed that he had been inhaling cannabis for about 7 to 8 years, his dependency had increased during the last 4 to 5 months, and he had used cannabis a few days before presenting to the ED. The patient had been smoking 15 cigarettes a day for about 10 years. He was previously diagnosed with hereditary neuropathy disease (Charcot-Marie-Tooth disease).
The neurologic examination revealed that his general condition was good, and he was conscious, cooperative, and oriented. His speech was natural. The cranial nerve examination was normal. Muscle strength was evaluated as bilateral upper extremity proximal 5/5, distal 4/5 and proximal lower extremity 4/5, distal 3/5. The patient’s foot and leg muscles were atrophic, and his gait was ataxic. In the sensory examination, loss of body temperature, touch, and proprioceptive sensations predominantly in the distal were observed in the 4 extremities. Deep tendon reflexes exhibited hypoactive bilateral plantar reflexes and were inattentive. Bilateral pes cavus deformity, atrophy in the lower extremity muscles, and drop foot were observed, and these symptoms were determined to be compatible with Charcot-Marie-Tooth disease.
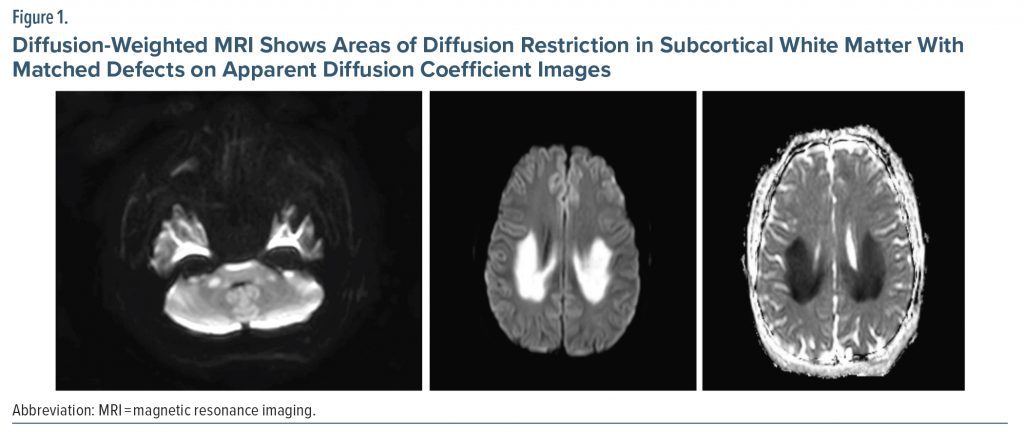
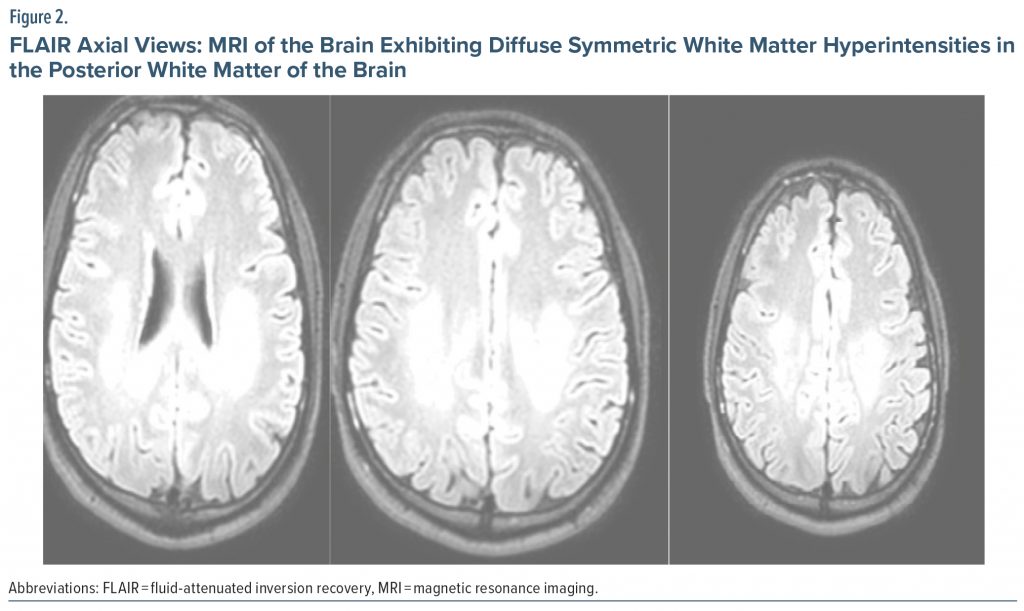
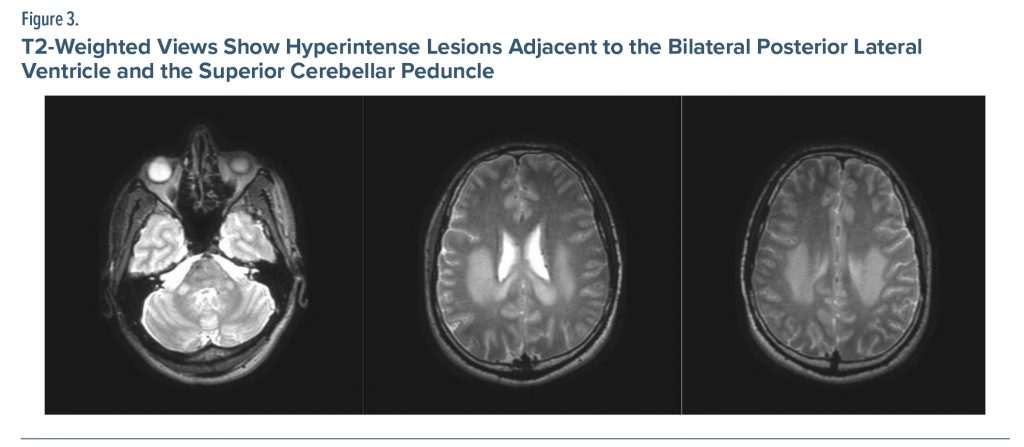
The patient’s complete blood count, vitamin B12, urinalysis, free T3 and T4, and thyroid-stimulating hormone tests were within normal limits. Antistreptolysin O, C-reactive protein, and sedimentation tests conducted to exclude infection were within normal limits. Vasculitis, torch, Lyme disease, brucella, hepatitis, HIV, and venereal disease research laboratory (for syphilis) tests were also unremarkable. Electromyography revealed sensorimotor polyneuropathy with diffuse axonal damage. Substance analysis revealed that his cannabinoid level was 183 ng/mL. Genetic evaluation for Charcot-Marie-Tooth disease was requested since the patient exhibited the previously mentioned symptoms, which was similar to his sibling. It was recommended to assess the Cmt-1 gene. The fluid-attenuated inversion recovery (FLAIR) and T2-weighted cranial MRI revealed white matter extending from the adjacent lateral ventricle posterior horn and occipital horn to the splenium and from the middle cerebellar peduncles and internal capsule hind legs to the brain stem, as well as hyperintense diffusion restriction (Figure 1, Figure 2, Figure 3). It was concluded that the current clinical and radiologic presentation of the patient could be considered as spongiform encephalopathy due to substance use. Treatment with prednisolone 10 mg/d was initiated. The patient received inpatient treatment in the neurology clinic for 3 days, and a psychiatrist was consulted. The patient was then transferred to the psychiatry clinic for addiction treatment.
Discussion
Leukoencephalopathy is characterized by cognitive, motor, sensory, and visual problems due to its effects on the cerebral white matter. The clinical properties of leukoencephalopathy could range from inattention, forgetfulness, and personality changes to dysarthria, ataxia, dementia, coma, and death.5 In previous studies,1–3 use of cocaine, methylenedioxymethamphetamine (MDMA or ecstasy), and heroin were associated with toxic leukoencephalopathy. Signal variations in the bilateral cerebral white matter posterior, cerebellar white matter, and posterior horn of the internal capsule are characteristics of cannabis-induced leukoencephalopathy in T2 and FLAIR-weighted imaging.6 It is known that marijuana, like heroin, has several adverse effects on the central nervous system and cognitive functions.7 The cerebral volumetric changes induced by cannabis in particular are also well known. In a study conducted in Turkey, it was observed that the hippocampus and amygdala volumes of individuals who abused cannabis for more than a decade decreased by 12% and 7%, respectively.8 Sporadic strokes observed in young cannabis smokers without a family history were suggested to be due to vasospasm.9 Patients having strokes while using cannabis and the absence of abnormal angiographic findings supported this suggestion.9 Another related mechanism is the irregularity of cerebral blood flow and postural hypotension after cannabis use. However, this mechanism is more important in patients with reduced cerebrovascular reserve. The vasculitic process has also been considered as a third mechanism, and this view was supported by the identification of cannabinoid arteritis, which is similar to Buerger’s disease.9 It is unknown whether the mechanisms responsible for cannabis-induced stroke also play a role in toxic encephalopathy associated with cannabis use. Our literature review revealed no cases of leukoencephalopathy associated with chronic marijuana use, thus further investigation into the possible mechanisms in toxic encephalopathy is warranted. This case of toxic encephalopathy associated with cannabis use contributes to the existing literature.
Article Information
Published Online: October 31, 2023. https://doi.org/10.4088/PCC.23cr03525
© 2023 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2023;25(6):23cr03525
Submitted: March 14, 2023; accepted July 21, 2023.
To Cite: Korkmaz S, Gülşen SÇ, Tatlı S, et al. Leukoencephalopathy after excessive cannabinoid use. Prim Care Companion CNS Disord. 2023;25(6):23cr03525.
Author Affiliations: Department of Psychiatry, Fırat University, Faculty of Medicine, Elazıg, Turkey (Korkmaz, Gülşen); Department of Neurology, Fırat University, Faculty of Medicine, Elazıg, Turkey (Tatlı, Aytaç); Department of Psychiatry, Elazig Mental Health and Diseases Hospital, Elazığ, Turkey (Kılıç, Kaya).
Corresponding Author: Sevda Korkmaz, MD, Department of Psychiatry, Fırat University Faculty of Medicine, Elazıg, Turkey ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Consent was received from the patient to publish the case report, and information has been de-identified to protect anonymity.
References (9)

- Sempere AP, Posada I, Ramo C, et al. Spongiform leucoencephalopathy after inhaling heroin. Lancet. 1991;338(8762):320. PubMed CrossRef
- Vosoughi R, Schmidt BJ. Multifocal leukoencephalopathy in cocaine users: a report of two cases and review of the literature. BMC Neurol. 2015;15(1):208. PubMed CrossRef
- Mu J, Li M, Guo Y, et al. Methamphetamine-induced toxic leukoencephalopathy: clinical, radiological and autopsy findings. Forensic Sci Med Pathol. 2017;13(3):362–366. PubMed CrossRef
- Riley DS, Barber MS, Kienle GS, et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol. 2017;89:218–235. PubMed CrossRef
- Filley CM, McConnell BV, Anderson CA. The expanding prominence of toxic leukoencephalopathy. J Neuropsychiatry Clin Neurosci. 2017;29(4):308–318. PubMed CrossRef
- Kumar Y, Drumsta D, Mangla M, et al. Toxins in brain! magnetic resonance (MR) imaging of toxic leukoencephalopathy - a pictorial essay. Pol J Radiol. 2017;82:311–319. PubMed CrossRef
- Pope HG Jr, Gruber AJ, Hudson JI, et al. Neuropsychological performance in long-term cannabis users. Arch Gen Psychiatry. 2001;58(10):909–915. PubMed CrossRef
- Yücel M, Solowij N, Respondek C, et al. Regional brain abnormalities associated with long-term heavy cannabis use. Arch Gen Psychiatry. 2008;65(6):694–701. PubMed CrossRef
- Mateo I, Pinedo A, Gomez-Beldarrain M, et al. Recurrent stroke associated with cannabis use. J Neurol Neurosurg Psychiatry. 2005;76(3):435–437. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!