Prim Care Companion CNS Disord 2023;25(2):22cr03309
To cite: Hanana F, Ettuveettil S, Moideen S, et al. Crowned dens syndrome masked as meningitis. Prim Care Companion CNS Disord. 2023;25(2):22cr03309.
To share: https://doi.org/10.4088/PCC.22cr03309
© 2023 Physicians Postgraduate Press, Inc.
aStarcare Hospital, Calicut, Kerala, India
bDepartment of Internal Medicine, Iqraa International Hospital and Research Centre, Calicut, Kerala, India
cDepartment of Psychiatry and Health Research, Iqraa International Hospital and Research Centre, Calicut, Kerala, India
*Corresponding author: N. A. Uvais, MBBS, DPM, Iqraa International Hospital and Research Centre, Malaparamba, Calicut, Kerala, 673009, India ([email protected]).
Dens, also known as odontoid process, is a bony protuberance from the second cervical vertebrae (axis). The first cervical vertebrae atlas pivots on the odontoid process of the axis.
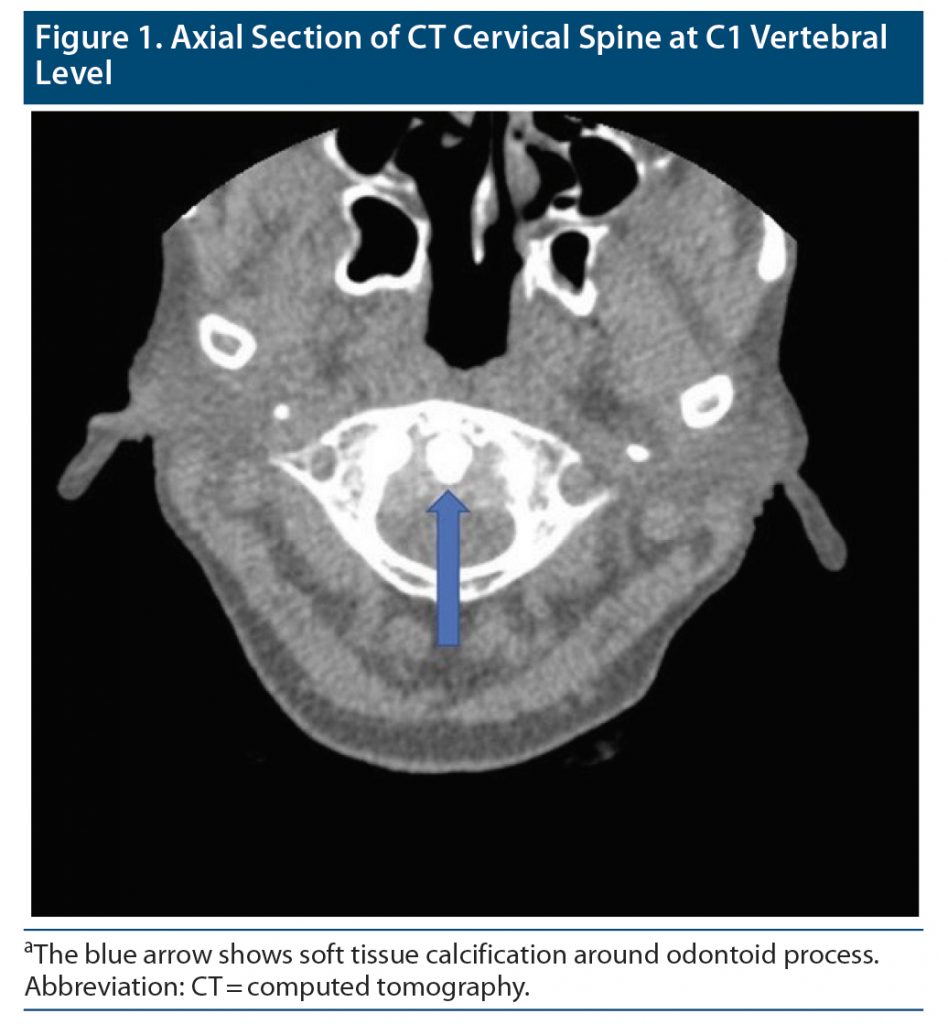
Crowned dens syndrome is a clinical and radiologic entity presenting with acute neck pain and specific radiographic findings of calcifications from calcium pyrophosphate dihydrate crystals superior to and surrounding the dens of the axis, resulting in a “crown-like” appearance on coronal views.1 Calcium pyrophosphate dihydrate crystal deposition is otherwise known as pseudogout. Crowned dens syndrome is an uncommon presentation of calcium pyrophosphate dihydrate deposition disease that manifests as acute attacks of neck pain with fever, neck rigidity, and elevated inflammatory markers due to radiodense deposits of calcium pyrophosphate dihydrate in ligaments around the odontoid process.2 Crowned dens syndrome is often misdiagnosed as trauma, meningitis, cervical discitis, or giant cell arteritis due to overlap of symptoms, which results in inappropriate invasive investigations such as lumbar puncture and subsequent treatment with parenteral broad-spectrum antimicrobial therapy.3 Here, we report a case of crowned dens syndrome that presented with acute neck pain in the emergency department and was initially suspected to be meningitis.
Case Report
A 64-year-old man with no premorbid conditions presented to the emergency department with a history of severe headache of 4 days duration. He also complained of neck pain and restricted neck movements due to the pain. There was no history of fever, vomiting, or cough. On examination, his vital signs were stable. Systemic examination revealed painful and restricted range of movement of the neck. There was tenderness at the cervical spine. Kernig’s sign was positive. Laboratory tests revealed C-reactive protein (CRP) of 36.3 mg/L. The 24-hour blood culture was sterile for both aerobic and anaerobic organisms. Computed tomography (CT) of the cervical spine showed mild retro-odontoid hypodense soft tissue thickening (Figure 1) and degenerative changes of the atlanto-dental joint with subchondral cysts and mild erosive changes due to chronic calcium pyrophosphate deposition. The patient was treated with colchicine, nonsteroidal anti-inflammatory drugs (NSAIDS), and steroids. He improved symptomatically and was discharged with follow-up on an outpatient basis.
Discussion
Calcium pyrophosphate dihydrate crystal deposition disease has varied clinical presentations based on the anatomic location of crystal deposition. Crystal deposition disease of the cervical spine frequently involves the odontoid process including the synovial membrane, articular capsule, transverse ligament, and transverse cruciate and alar ligaments.4 This rare condition known as crowned dens syndrome was first described by Bouvet et al1 in 1985 due to a crown-like appearance on coronal view. The prevalence of periodontoid calcification increases significantly in those aged ≥ 60 years.5 It also occurs more frequently in patients with pseudogout of the peripheral joints and in those with acute neck pain than in asymptomatic controls.5
While such calcification can often remain asymptomatic, it may present with acute neck pain due to nonspecific inflammatory reactions around the crystals.6 In a study by Salaffi et al,7 9 of the 49 cases of crystal deposit (18.4%) presented with neck symptoms. Acute neck pain can present with other manifestations such as meningism, cervico-brachial pain, and occipital and temporal headaches.7
Markers of inflammation such as increased body temperature, CRP levels, and white blood cell count may be present. CT is the gold standard for the detection of crystal deposition adjacent to the odontoid process.8 Nonenhanced CT will show calcifications in the periodontoid ligaments between the dens and the atlas. CT may also show soft tissue thickening and subchondral bone cyst formation and help eliminate alternative causes of neck pain.2 The crowned dens deposits could be due to either calcium pyrophosphate dihydrate or hydroxyapatite. Imaging findings cannot be used to differentiate between them. The definitive diagnosis is based on histologic study of the crystals.9
Once diagnosed correctly, crowned dens syndrome shows marked improvement in symptoms within days to weeks of treatment.4 First-line therapy for crowned dens syndrome aligns with that for pseudogout. NSAIDs are the mainstay of therapy. Colchicine is also frequently used. Patients who cannot tolerate NSAIDs or colchicine are usually started on low-dose corticosteroids.6,10 Risk factors for calcium pyrophosphate dihydrate disease such as hypomagnesemia, hyperparathyroidism, hypophosphatemia, and hemochromatosis should also be assessed.2 Rapid and correct diagnosis of crowned dens syndrome will prevent unnecessary and invasive investigations (lumbar puncture biopsy), inappropriate treatment (antibiotics and antiviral drugs), and prolonged hospitalization. Examples include a triad of headache, fever, and cervical morning stiffness, prompting a provisional diagnosis of meningitis and confirmatory lumbar puncture or cervical metastatic spondylitis in the case of a medical history of cancer.6 When cervical stiffness is associated with pain in the shoulder girdle and jaw claudication, crowned dens syndrome can be mistaken for polymyalgia rheumatica and/or giant cell arteritis, resulting in temporal artery biopsy and long-term steroid treatment.7
Crowned dens syndrome is an uncommon condition but is fairly amenable to treatment and is often mistaken for more common causes of fever and neck pain. Therefore, in elderly patients presenting with acute-onset neck pain/stiffness, fever, and features of systemic inflammation, crowned dens syndrome should be considered in the differentials to avoid invasive investigations and inappropriate treatment.
Published online: April 11, 2023.
Relevant financial relationships: None.
Funding/support: None.
Patient consent: Consent was received from the patient to publish the case report, and information has been de-identified to protect anonymity.
References (10)

- Bouvet JP, le Parc JM, Michalski B, et al. Acute neck pain due to calcifications surrounding the odontoid process: the crowned dens syndrome. Arthritis Rheum. 1985;28(12):1417–1420. PubMed CrossRef
- Ojemolon PE, Edigin E, Annapureddy N, et al. A case of acute neck pain: the crowned dens syndrome. Cureus. 2020;12(8):e9555. PubMed CrossRef
- Wu DW, Reginato AJ, Torriani M, et al. The crowned dens syndrome as a cause of neck pain: report of two new cases and review of the literature. Arthritis Rheum. 2005;53(1):133–137. PubMed CrossRef
- Goto S, Umehara J, Aizawa T, et al. Crowned dens syndrome. J Bone Joint Surg Am. 2007;89(12):2732–2736. PubMed CrossRef
- Kobayashi T, Miyakoshi N, Konno N, et al. Age-related prevalence of periodontoid calcification and its associations with acute cervical pain. Asian Spine J. 2018;12(6):1117–1122. PubMed CrossRef
- Koyfman A, Yaffe D. Crowned dens syndrome: a case report. Neuroradiol J. 2014;27(4):495–497. PubMed CrossRef
- Salaffi F, Carotti M, Guglielmi G, et al. The crowned dens syndrome as a cause of neck pain: clinical and computed tomography study in patients with calcium pyrophosphate dihydrate deposition disease. Clin Exp Rheumatol. 2008;26(6):1040–1046. PubMed
- Takahashi T, Tamura M, Takasu T, et al. Clinical and quantitative analysis of patients with crowned dens syndrome. J Neurol Sci. 2017;376:52–59. PubMed CrossRef
- Feydy A, Lioté F, Carlier R, et al. Cervical spine and crystal-associated diseases: imaging findings. Eur Radiol. 2006;16(2):459–468. PubMed CrossRef
- McCarron EP, Wilson J, Galkin S, et al. Crowned dens syndrome: an easily overlooked cause of fever and neck stiffness. QJM. 2020;113(1):52–53. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!