Mirtazapine is an antidepressant approved for the treatment of major depressive disorder but commonly prescribed off label for insomnia and anxiety because of its relatively benign safety profile and broad range of effects. It is a tetracyclic antidepressant drug that antagonizes the 5-hydroxytryptamine (5-HT2A), 5-HT2C, and 5-HT3 serotonin receptors along with α-2 adrenergic auto/ heteroreceptors, leading to an overall increase in adrenergic and serotonin activity.1 Side effects such as weight gain, drowsiness, constipation, and dry mouth are common.2 Ototoxicity is incredibly rare. It can manifest as a variety of symptoms, including hearing loss, tinnitus, or auditory hallucinations. It has only been reported twice in the literature, and the aforementioned triad was not fully present in either case.3,4 Furthermore, in both cases,3,4 ototoxic symptoms began shortly after initiation of the medication.
Here, we present the case of a patient suffering from hearing loss, tinnitus, and musical hallucinations following several months of mirtazapine use. Given the widespread use of mirtazapine, prescribers need to know how to manage medication-induced ototoxicity. Indeed, of drugs associated with ototoxicity, the second largest class is psychotropics.5
Case Report
The patient is a 57-year-old woman with a history of type II diabetes, anxiety treated with mirtazapine (45 mg nightly) started 7 months ago, opioid use disorder on methadone, and alcohol use disorder, who presented to the hospital with bilateral hearing loss that is worse on the left side. She was admitted to the medicine service for treatment of uncontrolled type II diabetes and hyperglycemic hyperosmolar state with polyuria and polydipsia. She has had hearing loss for 1 week, associated with new-onset tinnitus and auditory hallucinations (“like music in my ear”). The patient has no past or family history of hearing loss. She denies any vertigo, headaches, or trauma/infections preceding her symptoms. Besides electrolyte values and glucose levels consistent with hyperglycemic hyperosmolar state, the rest of the patientʼs medical workup (including vitals, complete blood count, kidney function, and drug levels) was unremarkable. The patient was not receiving any known ototoxic medications besides mirtazapine. Ear, nose, and throat consultation suggested this was the likely culprit, and audiograms were requested.5
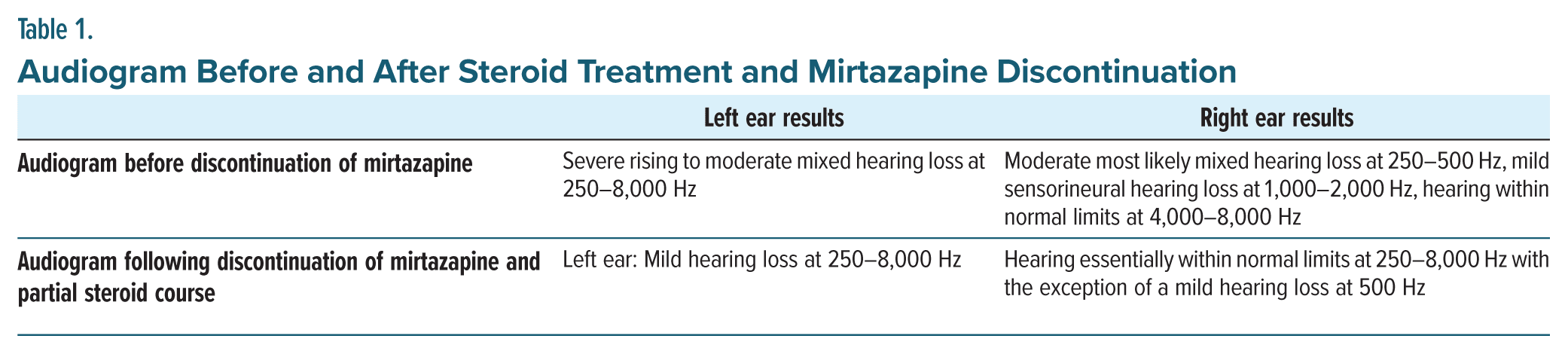
Mirtazapine was discontinued, and a 15-day steroid taper was started. The steroids were discontinued after 6 days due to worsening paranoia, hallucinations, and agitation that were suspected to be secondary to steroid-induced psychosis. Initial and final audiograms showed that her hearing loss and associated symptoms largely resolved even with this partial treatment (Table 1).
Discussion
This is the first report, to our knowledge, of mirtazapine-induced ototoxicity where the complete triad of hearing loss, tinnitus, and auditory hallucinations was present. Medication induced ototoxicity is posited to be due to various factors, including disruption of blood flow, damage to hair cells, and degeneration of the vestibulocochlear nerve.6 For mirtazapine, the specific mechanism is unknown. The treatment for all medication-induced ototoxicity is largely the same: discontinuation of the offending agent and then, depending on the severity, a short steroid course.7 Here, because of the debilitating nature of the patientʼs symptoms, the latter was opted for.
Interestingly, a prior report4 described this hearing loss as being “irreversible,” whereas our patient’s symptoms did improve. Additionally, this case was unique in that the symptoms started some months following initiation of the medication rather than immediately. This is surprising, as there would have been expected to be a progression of hearing-related symptoms following mirtazapine initiation or some additional environmental trigger such as trauma or infection causing sudden onset.
Further investigation is warranted, potentially involving animal or in vitro models to better understand the pathogenesis of this process given the lack of research into the mechanism of mirtazapine-related ototoxicity. In the meantime, clinicians should add mirtazapine to the existing list of psychotropics that can cause ototoxicity and lend caution to its use in patients at high risk for developing hearing impairment.
Article Information
Published Online: November 7, 2024. https://doi.org/10.4088/PCC.24cr03795
© 2024 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2024;26(6):24cr03795
Submitted: June 22, 2024; accepted August 20, 2024.
To Cite: Zhang V, Opler DJ. A side effect you’ve never heard of: ototoxicity associated with mirtazapine. Prim Care Companion CNS Disord. 2024;26(6):24cr03795.
Author Affiliations: Department of Psychiatry, Rutgers New Jersey Medical School, Newark, New Jersey (both authors).
Corresponding Author: Vincent Zhang, MPH, Department of Psychiatry, Rutgers New Jersey Medical School, 185 South Orange Ave, Newark, NJ 07103 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Informed consent was obtained from the patient to publish the case report, and information was de-identified to protect anonymity.
References (7)

- Alam A, Voronovich Z, Carley JA. A review of therapeutic uses of mirtazapine in psychiatric and medical conditions. Prim Care Companion CNS Disord. 2013;15(5):PCC.13r01525. PubMed CrossRef
- Anttila SA, Leinonen EV. A review of the pharmacological and clinical profile of mirtazapine. CNS Drug Rev. 2001;7(3):249–264. PubMed CrossRef
- Lee GH, Stewart JT. A case of musical hallucinations related to mirtazapine. Clin Neuropharmacol. 2018;41(6):222–223. PubMed CrossRef
- Dursun E, Akpinar A, Battal B. Sudden hearing loss associated with mirtazapine therapy: a case report. Klin Psikofarmakol Bul. 2009;19(4):417–419.
- Rizk HG, Lee JA, Liu YF, et al. Drug-induced ototoxicity: a comprehensive review and reference guide. Pharmacotherapy. 2020;40(12):1265–1275. PubMed CrossRef
- Ganesan P, Schmiedge J, Manchaiah V, et al. Ototoxicity: a challenge in diagnosis and treatment. J Audiol Otol. 2018;22(2):59–68. PubMed CrossRef
- Hammill TL, Campbell KC. Protection for medication induced hearing loss: the state of the science. Int J Audiol. 2018;57(suppl 4):S67–S75. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!