The identification of N-methyl-d-aspartate receptor (NMDAR)–antibody encephalitis (AE) recognized that some patients with rapidly progressive psychiatric/cognitive symptoms, seizures, abnormal movements, autonomic dysfunction, hypoventilation, and coma of unknown cause had an autoimmune disease. Tumors, usually ovarian teratoma (OT), are a known trigger of NMDAR autoimmunity.1,2
Pleomorphic in nature, psychosis and acute behavioral changes (ie, agitation, disorganized behavior) are the most frequently reported psychiatric manifestations of NMDAR-AE, although depressed level of consciousness and catatonia are also common.3 Importantly, about 80% of patients improve with immunotherapy and, if needed, tumor removal.2
We present a young woman who developed acute-onset behavioral changes accompanied by psychosis and catatonia, ultimately determined to have NMDAR-AE. Despite prompt treatment, symptoms progressed, including development of a minimally conscious state (MCS).
Case Report
Our patient, a 21-year-old woman with no prior psychiatric or medical history, presented to the emergency department due to “behavioral outbursts.” Four days prior to admission, the patient developed auditory hallucinations/delusions, disorganized speech, and agitation but had limited recall of autobiographical events over the preceding 2 weeks. Physical examination, including vital signs, was unremarkable. The patient denied alcohol and illicit substance use, and blood alcohol level/urine drug screen were both negative. We were consulted on admission to the medical unit.
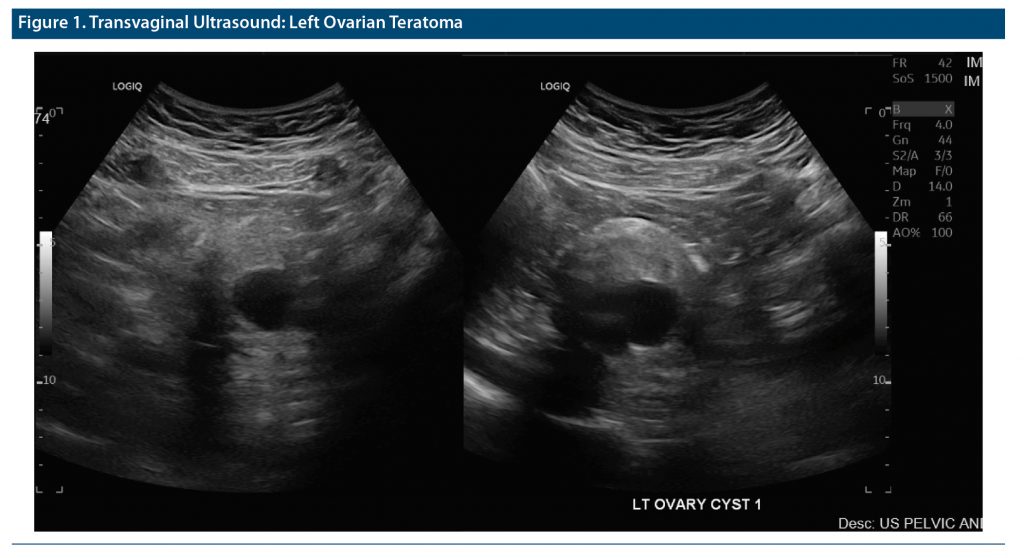
Our patient’s longitudinal course while hospitalized is summarized in Table 1,4–8 including symptoms, evaluation, treatment, and procedures. The transvaginal ultrasound results are provided in Figure 1. Ultimately confirmed by cerebrospinal fluid antibody positivity, our patient was treated for NMDAR-AE, initially with tumor excision and, subsequently, intravenous immunoglobulin (IVIg)/plasmapheresis. Eleven days after surgery, dexmedetomidine/other sedation was discontinued, yet our patient remained in a stupor for 6 additional days. Forthwith, all acute symptoms abated, with the patient developing the MCS. The latter ultimately resolved after 8 days of zolpidem treatment.
In the post-acute phase, our patient’s Montreal Cognitive Assessment7 score was 25 (5 points lost in short-term memory recall), and on hospital day 50, she was transferred to a rehabilitation facility, without immunotherapy but maintained on zolpidem.
Discussion
The frequency of NMDAR-AE in cases with OT involvement ranges from 30% to 60%.9 Furthermore, while autoimmune encephalitis is increasingly considered in patients with psychiatric symptoms, as it is potentially treatable with immunotherapy, autoimmune encephalitis is much less common than primary psychiatric disease, for instance, accounting for less than 1% of first episode of psychosis.10
At our initial evaluation, our patient’s illness had rapidly progressed to unresponsiveness with catatonic features. In addition, her acute onset (4 days) of psychosis with lack of prodromal symptoms of schizophrenia and lack of personal and family psychiatric/substance use history prompted our evaluation for possible nonpsychiatric/autoimmune etiologies.11 Despite uncovering our patient’s OT, female patients with OT-triggered NMDAR-AE reportedly account for only 1.17%–3.07% of OT patients.12,13
While our patient’s phenotype, save prodromal flu-like symptoms, was consistent with NMDAR-AE, her paraclinical features, save mild pleocytosis, were unremarkable.2 Interestingly, during its post-acute phase, neuropsychological dysfunction is experienced by most patients recovering from NMDAR-AE. Commonly observed deficits occur in the domains of episodic memory (as in our patient) and executive functioning.14
Finally, after treatment with IVIg/plasmapheresis, her unresponsiveness only progressed to the MCS, albeit without catatonic features. Yet, in the context of post-acute NMDAR-AE, zolpidem treatment for MCS was effective. In brief, zolpidem, a selective agonist at the ω1 subtype receptor of γ-aminobutyric acid–A receptor complex, has been posited to potentially aid in recovery of MCS by restoring normal function in frontocortico-striatopallidal-thalamocortical circuitry vis-a-vis inhibiting areas that are inhibitory.15,16
In conclusion, we believe our case emphasizes the importance for clinicians to consider (1) NMDAR-AE for those patients, especially female, with an acute and rapidly progressive pleomorphic psychiatric presentation and (2) the potential effect zolpidem can have on patients with MCS.
Article Information
Published Online: August 1, 2023. https://doi.org/10.4088/PCC.22cr03466
© 2023 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2023;25(4):22cr03466
Submitted: December 15, 2022; accepted February 17, 2023.
To Cite: Spiegel DR, Ahuja K, Reid FE, et al. A case of ovarian teratoma–induced N-methyl-d-aspartate receptor antibody encephalitis presenting with psychosis and catatonia, progressing to the minimally conscious state and successfully treated with adjunctive zolpidem. Prim Care Companion CNS Disord. 2023;25(4):22cr03466.
Author Affiliations: Department of Psychiatry and Behavioral Sciences, Eastern Virginia Medical School, Norfolk, Virginia (all authors).
Corresponding Author: David R. Spiegel, MD, Eastern Virginia Medical School, Department of Psychiatry and Behavior Sciences 825 Fairfax Avenue, Norfolk, VA 23507 ([email protected]).
Relevant Financial Relationships: Dr Spiegel is in the Speaker’s Bureau for Allergen, Alkermes, Otsuka, and IntraCellular, but has no conflict of interest in preparation of this manuscript. The remainder of the authors have no disclaimer/conflict of interest to report.
Funding/Support: There was no direct funding, other financial support (including drug company support), or material support received for this work.
Patient Consent: Consent was verbally received from the patient to publish the case report, and information has been de-identified to protect anonymity.
References (16)

- Al-Diwani A, Handel A, Townsend L, et al. The psychopathology of NMDAR-antibody encephalitis in adults: a systematic review and phenotypic analysis of individual patient data. Lancet Psychiatry. 2019;6(3):235–246. PubMed CrossRef
- Dalmau J, Armangué T, Planagumà J, et al. An update on anti-NMDA receptor encephalitis for neurologists and psychiatrists: mechanisms and models. Lancet Neurol. 2019;18(11):1045–1057. PubMed CrossRef
- Ford H, Griffith S, Warren N, et al. Psychiatric manifestations of autoimmune encephalitis. Autoimmun Rev. 2022;21(9):103145. PubMed CrossRef
- Bush G, Fink M, Petrides G, et al. Catatonia, I: rating scale and standardized examination. Acta Psychiatr Scand. 1996;93(2):129–136. PubMed CrossRef
- Ely EW, Truman B, Shintani A, et al. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS). JAMA. 2003;289(22):2983–2991. PubMed CrossRef
- Giacino JT, Kalmar K, Whyte J. The JFK Coma Recovery Scale-Revised: measurement characteristics and diagnostic utility. Arch Phys Med Rehabil. 2004;85(12):2020–2029. PubMed CrossRef
- Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699. PubMed CrossRef
- Ely EW, Gautam S, Margolin R, et al. The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Med. 2001;27(12):1892–1900. PubMed CrossRef
- Delangle R, Demeret S, Canlorbe G, et al. Anti-NMDA receptor encephalitis associated with ovarian tumor: the gynecologist point of view. Arch Gynecol Obstet. 2020;302(2):315–320. PubMed CrossRef
- Flanagan EP, Geschwind MD, Lopez-Chiriboga AS, et al. Autoimmune encephalitis misdiagnosis in adults. JAMA Neurol. 2023;80(1):30–39. PubMed CrossRef
- Pollak TA, Lennox BR, Müller S, et al. Autoimmune psychosis: an international consensus on an approach to the diagnosis and management of psychosis of suspected autoimmune origin. Lancet Psychiatry. 2020;7(1):93–108. PubMed CrossRef
- Wu CY, Wu JD, Chen CC. The association of ovarian teratoma and anti-N-methyl-d-aspartate receptor encephalitis: an updated integrative review. Int J Mol Sci. 2021;22(20):10911. PubMed CrossRef
- Li JH, Milla SS, Gombolay GY. Rate of anti-NMDA receptor encephalitis in ovarian teratomas. Neuropediatrics. 2022;53(2):133–135. PubMed CrossRef
- McKeon GL, Robinson GA, Ryan AE, et al. Cognitive outcomes following anti-N-methyl-D-aspartate receptor encephalitis: A systematic review. J Clin Exp Neuropsychol. 2018;40(3):234–252. PubMed CrossRef
- Bomalaski MN, Claflin ES, Townsend W, et al. Zolpidem for the treatment of neurologic disorders: a systematic review. JAMA Neurol. 2017;74(9):1130–1139. PubMed CrossRef
- Schiff ND. Recovery of consciousness after brain injury: a mesocircuit hypothesis. Trends Neurosci. 2010;33(1):1–9. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!