Delusional infestation (DI) is a psychiatric disorder characterized by self-induced cutaneous lesions. Patients maintain a persistent delusional belief that their body, particularly the skin, is infested with small pathogens, either living or non-living, despite a lack of dermatological or microbiological evidence.1–4 DI can present in various clinical forms, as classified by Le and Gonski5 and Hinkle.6 Table 1 outlines the 3 clinical subtypes of DI.
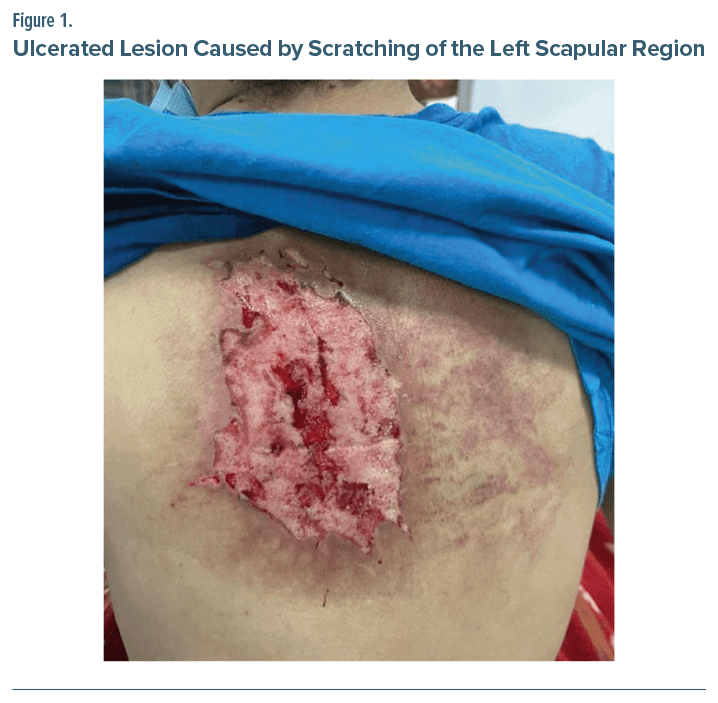
We present a case of secondary (organic) DI in a patient with a history of polysubstance use, including Δ9- tetrahydrocannabinol (THC), cocaine, lysergic acid diethylamide (LSD), 3,4- methylenedioxymethamphetamine (MDMA), phencyclidine (PCP), adrenochrome, and ethanol. The patient sought emergency care for a severe cutaneous lesion in the left scapular region.
Case Report
A 20-year-old man with a 5-year history of polysubstance use (THC, cocaine, LSD, MDMA, PCP, adrenochrome, and alcohol) presented to the emergency department in August 2024 with a severe pruritic lesion in the left scapular region. Examination revealed a well demarcated ulcerated lesion with a perilesional erythematous halo measuring 30 × 30 cm, caused by excessive scratching (Figure 1). Over the past 22 days, the patient had been compulsively scratching due to delusions of “bugs eating his skin,” which led to self-inflicted injuries, and he occasionally ingested the scabs.
The patient had no prior history of mental disorders. He was admitted with a diagnosis of secondary (organic) DI and was treated with olanzapine 20 mg/d. A urine toxicology screen was positive for THC and benzodiazepines. The patient exhibited severe benzodiazepine withdrawal symptoms (Clinical Institute Withdrawal Assessment Scale-Benzodiazepines8 score: 40), and diazepam 10 mg was administered until the withdrawal symptoms were controlled.
Daily wound care with silver sulfadiazine, vitamin A, and lidocaine cream was provided as recommended by plastic surgery and dermatology consultation, with no antibiotics required per internal medicine. After detoxification and resolution of his psychotic symptoms, the patient no longer believed that he was infested with parasites and was transferred to a rehabilitation center for further care.
Discussion
DI is a complex psychiatric and dermatological disorder characterized by challenges in both diagnosis and treatment. It can present as a primary somatic-type delusional disorder or secondary to other psychiatric conditions, medical diseases, or substance abuse. The disorder typically progresses from a cutaneous sensory misinterpretation to tactile hallucinations, eventually solidifying into a fixed delusional belief. In cases of substance-induced DI, the abrupt onset and transient nature of symptoms—lasting hours, days, or weeks—complicates the clinical picture.9–12
This case underscores the importance of close collaboration between dermatologists and psychiatrists for accurate diagnosis and timely psychodermatologic intervention. Atypical antipsychotics, such as risperidone and olanzapine, are considered first-line treatments,13–16 particularly because of their ability to reduce dopamine levels in the striatum, which is believed to sustain the delusional state.17 In secondary DI, treatment should address any underlying comorbidities. Prognosis largely depends on the promptness of diagnosis and the initiation of appropriate interventions, with good outcomes observed in most cases when treated early.18 Addressing both substance use and psychotic symptoms is crucial for improving patient outcomes, especially in cases in which symptoms may become chronic, makingmanagement more challenging and potentially leading to treatment resistance.
Article Information
Published Online: April 22, 2025. https://doi.org/10.4088/PCC.24cr03887
© 2025 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2025;27(2):24cr03887
Submitted: November 5, 2024; accepted January 14, 2025.
To Cite: Torales J, Kunihiro D, López N, et al. Secondary delusional infestation in a male with a history of polysubstance use. Prim Care Companion CNS Disord 2025;27(2):24cr03887.
Author Affiliations: Department of Psychiatry, School of Medical Sciences, Universidad Nacional de Asunción, San Lorenzo, Paraguay (Torales, Kunihiro, López, Melgarejo, O’Higgins); School of Health Sciences, Universidad Sudamericana, Pedro Juan Caballero, Paraguay (Torales, Barrios); Department of Biostatistics, School of Medical Sciences, Santa Rosa del Aguaray Branch, Universidad Nacional de Asunción, Santa Rosa del Aguaray, Paraguay (Barrios).
Corresponding Author: Iván Barrios, PhD, Department of Biostatistics, School of Medical Sciences, Santa Rosa del Aguaray Branch, Universidad Nacional de Asunción, Avenida Primeros Concejales casi 11 de Septiembre, Santa Rosa del Aguaray, Paraguay ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Written and informed consent was received from the patient to publish this case report and photo, and information was de-identified to protect anonymity.
References (18)

- Torales J, García O, Barrios I, et al. Delusional infestation: clinical presentations, diagnosis, and management. J Cosmet Dermatol. 2020;19(12):3183–3188.
- Heller MM, Wong JW, Lee ES, et al. Delusional infestations: clinical presentation, diagnosis and treatment. Int J Dermatol. 2013;52(7):775–783. CrossRef
- Koo J, Lebwohl A. Psychodermatology: the mind and skin connection. Am Fam Physician. 2001;64(11):1873–1878.
- Torales J, González L, Ruiz Díaz C, et al. Delirio de infestación [Delusional Infestations]. In: Torales J, Malatesta E, eds. Psicodermatología: una actualización diagnóstica y terapéutica de las entidades clínicas más frecuentes [Psychodermatology: a diagnostic and therapeutic update of the most frequent clinical entities]. 1st edn. EFACIM; 2019:62–79.
- Le L, Gonski PN. Delusional parasitosis mimicking cutaneous infestation in elderly patients. Med J Aust. 2003;179(4):209–210. CrossRef
- Hinkle NC. Ekbom syndrome: the challenge of “invisible bug” infestations. Annu Rev Entomol. 2010;55:77–94. CrossRef
- Al-Imam AML. A systematic literature review on delusional parasitosis. J Dermatol Dermatol Surg. 2016;20:5–14. CrossRef
- Busto UE, Sykora K, Sellers EM. A clinical scale to assess benzodiazepine withdrawal. J Clin Psychopharmacol. 1989;9(6):412–416. CrossRef
- Revelli C, Pichon M, Cambazard F, et al. Consultation dermato-psychiatrique [Dermato-psychiatric consultation]. Ann Dermatol Venereol. 2002;129(5 Pt 1):742–745.
- Freudenmann R, Lepping P. Delusional infestation. Clin Microbiol Rev. 2009;22(4):690–732. CrossRef
- Vulink NC. Delusional infestation: state of the art. Acta Derm Venereol. 2016;96(217):58–63.
- Reich A, Kwiatkowska D, Pacan P. Delusions of parasitosis: an update. Dermatol Ther. 2019;9(4):631–638. CrossRef
- Freudenmann RW, Lepping P. Second-generation antipsychotics in primary and secondary delusional parasitosis: outcome and efficacy. J Clin Psychopharmacol. 2008;28(5):500–508.
- Lepping P, Russell I, Freudenmann RW. Antipsychotic treatment of primary delusional parasitosis: systematic review. Br J Psychiatry. 2007;191:198–205.
- Torales J, Melgarejo O, González I, et al. Psychopharmacology in dermatology: treatment of primary psychiatric conditions in dermatology. Dermatol Ther. 2020;33(4):e13557.
- Campbell EH, Elston DM, Hawthorne JD, et al.Diagnosis and management of delusional parasitosis. J Am Acad Dermatol. 2019;80(5):1428–1434. CrossRef
- Huber M, Karner M, Kirchler E, et al. Striatal lesions in delusional parasitosis revealed by magnetic resonance imaging. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(8):1967–1971. CrossRef
- Torales J, Almirón-Santacruz J, Barrios I, et al. “Cocaine bugs”: implications for primary care providers. Prim Care Companion CNS Disord. 2022;24(2):21cr03019.
Enjoy this premium PDF as part of your membership benefits!