Arrhythmogenic right ventricular dysplasia/ cardiomyopathy (ARVD/C) is an inherited cardiomyopathy characterized by the progressive replacement of the myocardium in the right ventricle with fibrofatty tissue that can foster cardiac arrhythmias and heart failure.1 Once a diagnosis of ARVD/C is established, an important management decision is whether to place an implantable cardioverter defibrillator (ICD) for treatment of sustained ventricular arrhythmias (VA) and prevention of sudden cardiac death (SCD). ARVD accounts for 3%–4% of deaths in sports and 5% of SCDs in those younger than age 65 years.2 As such, in a recent meta-analysis, the mean age of ICD implantation for primary or secondary prevention of SCD was 40 years old,3 although studies have demonstrated a favorable long-term prognosis in properly treated patients.2 Thus, given the early age of ICD implantation, patients are typically exposed to many years of repeated ICD firings with associated medical/psychiatric challenges.4
We present the case of a patient with ARVD/C, post electrical storm from her ICD, who developed shock anxiety (SA) with phobic avoidance. While SA and posttraumatic stress disorder (PTSD) in patients with an ICD have been well documented in the literature,5–8 there is a paucity of evidence describing both the phenomenology of SA and psychiatric/psychological interventions for patients with ARVD/C-induced VA.4 The goal of this report is to extend the existing evidence in this population.
Case Report
The patient was a 63-year-old woman with a history of ARVD/ C-induced VA, who was status post ICD for 10 years with no complications or shocks. On the day of admission, the patient reported 3 days of nonadherence to scheduled metoprolol and subsequently developed 5 high-rate ventricular events for 6–12 seconds each. Upon admission to the hospital, the patient was hemodynamically stable, although sympathicolysis, sedation, and antiarrhythmic therapy were initiated with propranolol, diazepam, and amiodarone, respectively. Except for nonadherence to metoprolol, trigger identification and optimization was generally benign, including an unremarkable complete blood count, complete metabolic profile (including potassium and magnesium), blood alcohol, urine drug screen, troponin I, and infectious evaluation. Electrocardiogram demonstrated no evidence of ischemia or QTc interval prolongation with a stable echocardiogram/left ventricular ejection fraction of 60%. The patient had no changes in her emotional state, acute concomitant disease, or surgery. After ICD interrogation, there were no device/lead defects.
In an attempt to reduce the frequency of shock episodes, an electrophysiologist “reprogrammed” the patient’s ICD, with programming strategies including prolonged detection duration (30 of 40 ventricular beats) and increased heart rate threshold of tachycardia detection (182 beats/min) and using supraventricular detection discrimination algorithms and antitachycardia pacing (ATP). The detection duration was moderately extended, using fast-rate cutoffs, ATP in faster rate zones, and existing supraventricular tachycardia discrimination algorithms.
Three months after this hospitalization, the patient was referred to psychiatry for “progressive inability to leave her home” due to SA. The patient reported no prior psychiatric or substance/alcohol use history until the series of above events. She reported that in addition to ICD shocks, she developed a “panic attack,” including chest pain, shortness of breath, tachycardia, tremors, paresthesias, and feelings she was “going to die.” The patient stated that since the occurrence of index ICD shocks, she was no longer engaging in mild cardiologist prescribed exercise. Additionally, she avoided any activity that could result in the ICD shocks, which included not leaving her home or driving. Thus, she worked remotely. Furthermore, she was also hypervigilant about emotional symptoms, adding that she was anxious about developing any anxiety for concerns that this would lead to ICD shocks. The patient scored a 33 (maximum score of 50) and 30 on the Florida Shock Anxiety Scale9 (FSAS) and Posttraumatic Stress Disorder Checklist: Civilian Scale10 (PCL-C) (range, 17–85), respectively. Alternatively, the patient denied symptoms of major depressive disorder, mania, auditory/ visual hallucinations, delusions, or lethality. The mental status examination was remarkable for an anxious mood, although affect was appropriate. The remainder of the mental status examination was unremarkable, including speech and thought process. The patient’s Mini-Mental State Examination11 score was 30/30.
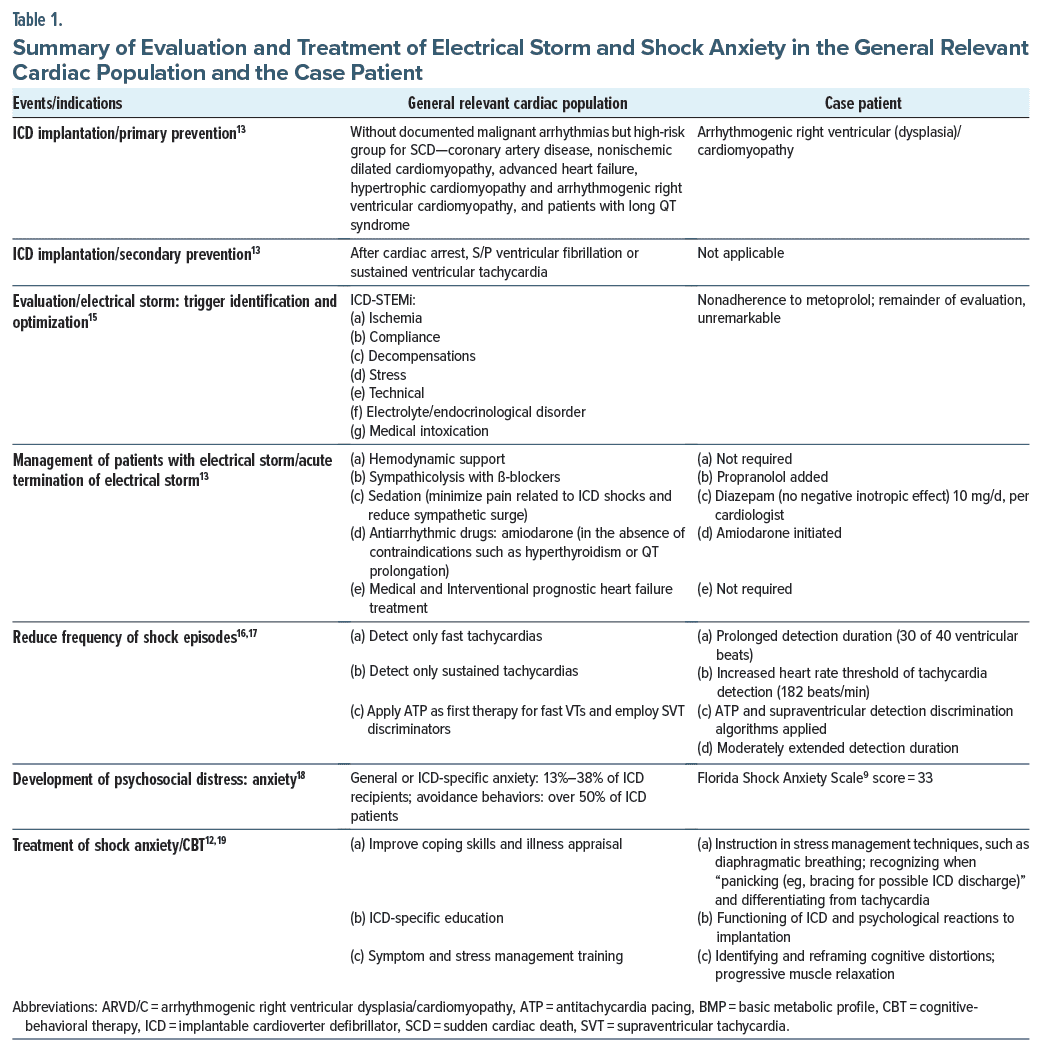
The patient began cognitive behavioral therapy (CBT), which involved psychoeducation, both about the ICD device and the psychological reactions to ICD implantation, as well as stress management techniques, wherein physical, cognitive, and behavioral functioning were delineated and individually targeted. Relaxation strategies (eg, progressive muscle relaxation) were taught to address physical manifestations of anxiety, and a cognitive component of treatment was taught to identify automatic negative thoughts (cognitive distortions) and challenge/ replace them with adaptive and accurate ones, utilizing a daily thought record to assist in the regular use of these cognitive skills. The patient was instructed to conceptualize the ICD as a foundation of safety from which she could re-engage in desired activities, rather than a source of threat that constrains the latter. She started a systematic desensitization protocol to expose emotions, thoughts, and activities that she feared, and a shock management plan was developed, including when to seek medical attention and utilizing the above CBT techniques post shock.12 After the conclusion of treatment, the patient’s FSAS score was 14 and PCL-C score was 24. Table 19,12–19 provides a summary of cardiac and psychiatric evaluation and treatment.
Discussion
Individuals with ARVD/C have a high ICD discharge rate. For instance, case series have reported an appropriate ICD discharge rate for treatment of a sustained ventricular arrhythmia of 50%–80%.4 Similar to the patient presented here, previous studies suggest that a relatively large proportion of the ICD population (20%–84%) experience SA, which has similarities to panic/phobic anxiety and has been well described.20 Furthermore, while not all studies support the relationship between ICD shocks and anxiety,4 converging evidence estimates >5 shocks over the lifetime significantly increases the risk of anxiety.7 Our patient experienced a total of 9 shocks during a 2-hour period after she developed 5 high-rate ventricular events. Additionally, in 1 study,21 in patients with ICDs, panic disorder and/or agoraphobia were identified in 16.7% of the patients. The prevalence of these diagnoses in those who did and did not experience ICD shock was 21% and 6.9%, respectively.21
Shock experience and female sex serve as potential risk factors for poor quality of life in ARVD/C patients.22 Over time, the former can be a predictor of phobic and anxiety disorders. Furthermore, shock storms, the precipitant of SA in our patient, have been reported to significantly increase anxiety levels in patients with an ICD, from 24% to 34%.23 Thus, shocks in ARVD/C patients should be treated as a “critical event,” warranting clinical attention. Reports indicate that this cohort might benefit from assessment of anxiety symptoms (ie, worry about future shock/ avoidance/hypervigilance to bodily sensations) following ICD shock to mitigate its effect on overall psychosocial functioning.1
Diagnosis of a cardiac genetic disorder with its symptomatic status, uncertainty regarding disease progression, risk of SCD, recommended lifestyle changes (ie, activity restrictions or career change), and genetic transmission to offspring all contribute to the potential psychological burden of disease. Studies on these disorders have consistently shown an elevated risk for anxiety; however, most of the relevant literature on this topic focuses on 2 of the most common genetic cardiac diseases, hypertrophic cardiomyopathy and inherited long QT syndrome.24 In fact, we were only able to retrieve 1 article on psychosocial aspects of ARVD/C.4
Independent of underlying diagnosis, patients requiring ICDs commonly experience anxiety related to the anticipation of a potential shock. While our patient was prescribed diazepam for sympatholysis during ICD electrical storm, her FSAS score was markedly elevated. Unfortunately, except for 1 study reporting the successful use of paroxetine with a behavioral component,25 there is a dearth of evidence for antidepressant efficacy in SA in patients with or without ARVD/C. That stated, we employed a CBT intervention, largely supported by prior studies and case reports,12,19,26–29 although not specifically in ARVD/C patients. Notably, we did not feel our patient endorsed syndromic PTSD, both clinically and scoring 30 on the PCL-C.
CBT in this cohort involved teaching techniques to improve coping skills and illness appraisal, such as developing a shock plan and strategies to reduce negative thoughts.24 Nonetheless, as psychosocial outcomes in those with ARVD/C are in its infancy, the literature is practically devoid of reports of using CBT for those with SA and ARVD/C. Thus, our case report is novel vis-a-vis further expanding the evidence on the development of SA in those with ARVD/C and an ICD, as well as utilizing CBT as primary treatment.
Despite our enthusiasm with the patient’s treatment response, there were limitations. For instance, the patient was prescribed 2 medications, diazepam and propranolol, that have demonstrated efficacy, albeit mixed, in the treatment of anxiety disorders with phobic avoidance.30,31 Thus, we cannot conclusively state that the patient would not have responded to diazepam and propranolol without CBT. Again, with mixed evidence, combination pharmacologic and CBT treatment has been proposed to result in a synergistic response as compared to monotherapy in anxiety disorders; thus, it would be difficult to determine how much of our patient’s response was due to medications, CBT, and/or a potential synergistic response.32–34
In closing, with the aforementioned CBT intervention, the patient’s FSAS score significantly decreased, and she was able to return to her social, occupational, and recreational activities, albeit with much restriction on exercise due to her underlying ARVD/C. Notably, most patients with ARVD/C-induced ventricular tachycardia adapt well to insertion of an ICD.22 For those, however, that develop SA, we recommend a program of CBT, demonstrated to lower moderate-high SA in patients after ICD insertion. Furthermore, based on this case, CBT seems to be an effective and safe treatment in ICD-induced SA in ARVD/C, although larger trials to validate these results are warranted.23
Article Information
Published Online: April 24, 2025. https://doi.org/10.4088/PCC.24cr03869
© 2025 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2025;27(2):24cr03869
Submitted: October 11, 2024; accepted January 9, 2025.
To Cite: Spiegel DR, Eckstrom A. Shock anxiety after electrical storm ventricular tachyarrhythmias treated with cognitive-behavioral therapy. Prim Care Companion CNS Disord 2025;27(2):24cr03869.
Author Affiliations: Department of Psychiatry and Behavioral Sciences, Eastern Virginia Medical School, Norfolk, Virginia (Spiegel, Eckstrom).
Corresponding Author: David R. Spiegel, MD, Department of Psychiatry and Behavior Sciences, Eastern Virginia Medical School, 825 Fairfax Ave, Norfolk, VA 23507 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Consent was received verbally from the patient to publish the case report, and information has been de-identified to protect anonymity.
References (34)

- Rhodes AC, Murray B, Tichnell C, et al. Quality of life metrics in arrhythmogenic right ventricular cardiomyopathy patients: the impact of age, shock and sex. Int J Cardiol. 2017;248:216–220. PubMed CrossRef
- Anderson EL. Arrhythmogenic right ventricular dysplasia. Am Fam Physician. 2006;73(8):1391–1398.
- Schinkel AFL. Implantable cardioverter defibrillators in arrhythmogenic right ventricular dysplasia/ cardiomyopathy: patient outcomes, incidence of appropriate and inappropriate interventions, and complications. Circ Arrhythm Electrophysiol. 2013;6(3):562–568. PubMed CrossRef
- James CA, Tichnell C, Murray B, et al. General and disease-specific psychosocial adjustment in patients with arrhythmogenic right ventricular dysplasia/ cardiomyopathy with implantable cardioverter defibrillators: a large cohort study. Circ Cardiovasc Genet. 2012;5(1):18–24. PubMed CrossRef
- Sears SF, Harrell R, Sorrell A, et al. Addressing PTSD in implantable cardioverter defibrillator patients: state-of-the-art management of ICD shock and PTSD. Curr Cardiol Rep. 2023;25(9):1029–1103.
- Freedenberg V, Thomas SA, Friedmann E. Anxiety and depression in implanted cardioverter-defibrillator recipients and heart failure: a review. Heart Fail Clin. 2011;7(1):59–68. PubMed CrossRef
- Schulz SM, Massa C, Grzbiela A, et al. Implantable cardioverter defibrillator shocks are prospective predictors of anxiety. Heart Lung. 2013;42(2):105–111. PubMed CrossRef
- Jacq F, Foulldrin G, Savouré A, et al. A comparison of anxiety, depression and quality of life between device shock and nonshock groups in implantable cardioverter defibrillator recipients. Gen Hosp Psychiatry. 2009;31(3):266–273.
- Kuhl E, Dixit N, Walker R, et al. Measurement of patient fears about implantable cardioverter defibrillator shock: an initial evaluation of the Florida Shock Anxiety Scale. Pacing Clin Electrophysiol. 2006;29(6):614–618. PubMed CrossRef
- Lang AJ, Wilkins K, Roy-byrne PP, et al. Abbreviated PTSD Checklist (PCL) as a guide to clinical response. Gen Hosp Psychiatry. 2012;34(4):332–338. PubMed CrossRef
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. PubMed CrossRef
- Hirsh AT, Sears SF, Jr, Conti JB. Cognitive and behavioral treatments for anxiety and depression in a patient with an implantable cardioverter defibrillator (ICD): a case report and clinical discussion. J Clin Psychol Med Settings. 2009;16(3):270–279. PubMed CrossRef
- Karczewska O, Młynarska A. Factors that cause concerns after cardioverter defibrillator implantation. Int J Environ Res Public Health. 2021;18(11):6095. CrossRef
- Israel CW, Barold SS. Electrical storm in patients with an implanted defibrillator: a matter of definition. Ann Noninvasive Electrocardiol. 2007;12(4):375–382. PubMed CrossRef
- Kleemann T, Lampropoulou E, Kouraki K, et al. Management of implantable cardioverter-defibrillator patients with appropriate ICD shocks: a 3-step treatment concept. Heart Rhythm O2. 2021;2(5):537–540. CrossRef
- Stevenson WG, John RM. Ventricular arrhythmias in patients with implanted defibrillators. Circulation. 2011;124(16):e411–e414.
- Wilkoff BL, Williamson BD, Stern RS, et al. Strategic programming of detection and therapy parameters in implantable cardioverter defibrillators reduces shocks in primary prevention patients: results from the PREPARE (Primary Prevention Parameters Evaluation) study. J Am Coll Cardiol. 2008;52(7):541–550.
- Ghezzi ES, Sharman RLS, Selvanayagam JB, et al. Burden of mood symptoms and disorders in implantable cardioverter defibrillator patients: a systematic review and meta-analysis of 39954 patients. Europace. 2023;25(6):euad130.
- Urizar GG, Sears SF, Handberg E, et al. Psychosocial intervention for a geriatric patient to address fears related to implantable cardioverter defibrillator discharges. Psychosomatics. 2004;45(2):140–144. PubMed CrossRef
- Morken IM, Isaksen K, Karlsen B, et al. Shock anxiety among implantable cardioverter defibrillator recipients with recent .tachyarrhythmia. Pacing Clin Electrophysiol. 2012;35(11):1369–1376. PubMed CrossRef
- Borne RT, Varosy PD, Masoudi FA. Implantable cardioverter-defibrillator shocks: epidemiology, outcomes, and therapeutic approaches. JAMA Intern Med. 2013;173(10):859–865. PubMed CrossRef
- de Ornelas Maia AC, Soares-Filho G, Pereira V, et al. Psychiatric disorders and quality of life in patients with implantable cardioverter defibrillators: a systematic review. Prim Care Companion CNS Disord. 2013;15(2):PCC.12r01456.
- Qintar M, George JJ, Panko M, et al. A prospective study of anxiety in ICD patients with a pilot randomized controlled trial of cognitive behavioral therapy for patients with moderate to severe anxiety. J Interv Card Electrophysiol. 2015;43(1):65–75. PubMed CrossRef
- Day SM. Anxiety in patients with arrhythmogenic right ventricular cardiomyopathy and implantable cardioverter defibrillators. Circ Cardiovasc Genet. 2012;5(1):2–4. PubMed CrossRef
- Kuijpers PM, Honig A, Wellens HJ. Effect of treatment of panic disorder in patients with frequent ICD discharges: a pilot study. Gen Hosp Psychiatry. 2002;24(3):181–184. PubMed CrossRef
- Pedersen SS, van den Broek KC, Sears SF. Psychological intervention following implantation of an implantable defibrillator: a review and future recommendations. Pacing Clin Electrophysiol. 2007;30(12):1546–1554. PubMed CrossRef
- Sears SF, Sowell LD, Kuhl EA, et al. The ICD shock and stress management program: a randomized trial of psychosocial treatment to optimize quality of life in ICD patients. Pacing Clin Electrophysiol. 2007;30(7):858–864. PubMed CrossRef
- Fitchet A, Doherty PJ, Bundy C, et al. Comprehensive cardiac rehabilitation programme for implantable cardioverter-defibrillator patients: a randomised controlled trial. Heart (British Card Soc). 2003;89(2):155–160. PubMed CrossRef
- Kohn CS, Petrucci RJ, Baessler C, et al. The effect of psychological intervention on patients’ long-term adjustment to the ICD: a prospective study. Pacing Clin Electrophysiol. 2000;23(4 Pt 1):450–456. PubMed CrossRef
- Whitehead WE, Blackwell B, Robinson A. Effects of diazepam on phobic avoidance behavior and phobic anxiety. Biol Psychiatry. 1978;13(1):59–64. PubMed
- Hede V, Devillé C. Treating psychiatric symptoms and disorders with non-psychotropic medications. Dialogues Clin Neurosci. 2019;21(2):193–201.
- Marshall RD, Cloitre M. Maximizing treatment outcome in post-traumatic stress disorder by combining psychotherapy with pharmacotherapy. Curr Psychiatry Rep. 2000;2(4):335–340. PubMed CrossRef
- Bandelow B, Reitt M, Röver C, et al. Efficacy of treatments for anxiety disorders: a meta-analysis. Int Clin Psychopharmacol. 2015;30(4):183–192.
- Bandelow B, Seidler-Brandler U, Becker A, et al. Meta-analysis of randomized controlled comparisons of psychopharmacological and psychological treatments for anxiety disorders. World J Biol Psychiatry. 2007;8(3):175–187. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!