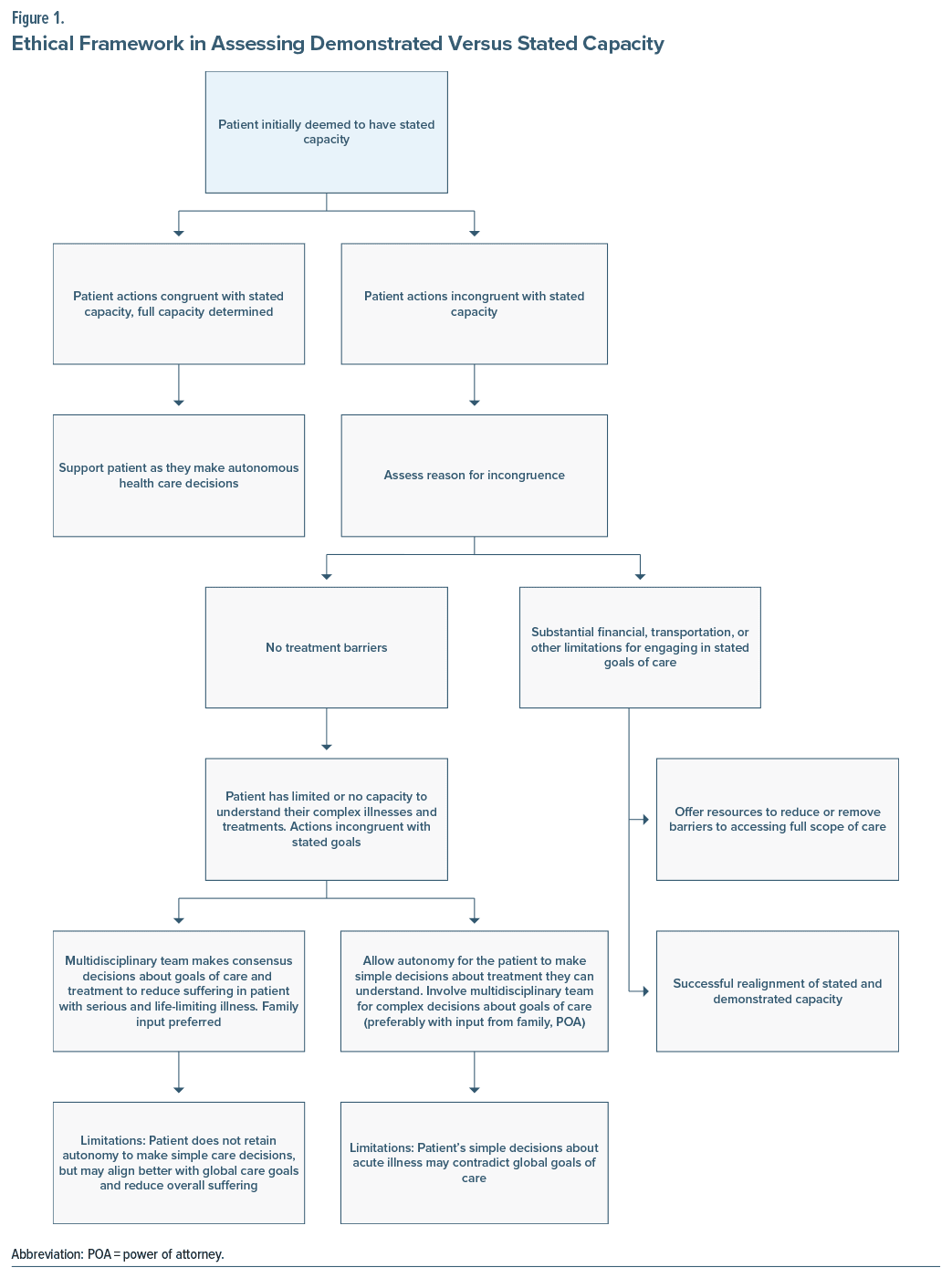
Medical ethical decisions are an integral part of a physician’s professional responsibilities and are foundational to quality patient-centered care. Often, there are complex patient cases that challenge even the most finely attuned ethical reasoner. Appelbaum and Grisso’s1 criteria for decisional capacity assessment include communicating a consistent choice, understanding the relevant information, appreciating the circumstances and consequences, and rationally manipulating the information. However, critics have pointed out that these criteria can be overtly “cognitive” and not fully attuned to the patient’s values and authenticity.2 Authenticity is an idea that someone is deciding while “not their self” or that it is the “illness speaking.”3 Difficulties can arise when the patient’s behaviors consistently contradict their stated decisions when determined to have decisional capacity. We present a complex case involving a patient with HIV, wherein decisional capacity was questioned based on the patient’s stated versus demonstrated capacity, which previously has not been described in the literature. Additionally, we propose a flowchart that clinicians can use when involved in such ethically challenging situations.
Case Report
A 52-year-old woman with a history of HIV encephalopathy (CD4 count 140 cells/mL [reference range, 500–1,500 cells/mL]), heart failure, and gastrostomy tube (G-tube) dependency presented to the emergency department from a nursing facility for worsening abdominal pain and combativeness. She was admitted for the treatment of an opportunistic abdominal infection and concerns for splenic abscess.
Upon evaluation, the patient was alert and oriented, and there was no evidence of any overt mood disorder or psychosis. She demonstrated limited insight into her disease burden. When the patient was asked about the transition to hospice and goals of care, she expressed that she wanted the full scope of treatment for her HIV and desired to prolong her life. However, it was discovered that the patient had a well-documented multiyear history of refusing HIV medications, leading to significant HIV disease progression and repeat hospitalizations. Per the patient’s sister, her power of attorney (POA), the patient was suffering greatly due to continued cycles of hospitalization, which was inconsistent with the patient’s values. Consequently, the patient’s POA had decided during the 2 previous hospitalizations to discontinue HIV medications and pursue hospice care. Consequently, the patient’s statement to pursue continued HIV treatment raised concerns about her capacity based on her stated goals, versus longstanding values and consistent treatment refusal. The patient went on to express that she desired to be discharged to a hotel after the current hospitalization, demonstrating poor insight into the severity of her global health state, while contradicting her stated desire to continue full treatment, which would require a nursing facility.
A multidisciplinary team meeting was held with the general medical team, psychiatry, palliative care, and the ethics consultation service. We arrived at the consensus that the patient had limited capacity to make simple decisions in the context of acute illness (desire to be pain free) but did not fully appreciate the totality of her health state, which is comprised of all the comorbidities at the specific trajectory and severity of each illness state (advanced AIDS and advanced heart failure). We determined that the patient had exhausted all benefits from curative treatments for advanced HIV disease, and all providers’ recommended palliative and hospice care for the management of her symptoms. The patient’s POA was notified of the recommendation for palliative and hospice care, and her POA was in agreement with this treatment plan. The patient was informed that she would be discharged to her skilled nursing facility under the care of hospice via a collective meeting with the primary team and her sister (POA). She was agreeable with the plan to prioritize comfort and reduce pain. All of her medications (eg, intravenous antibiotics) were discontinued prior to discharge except for her comfort medications. She was successfully transferred back to her skilled nursing facility via ambulance. She presented to the emergency department 13 days later with a dislodged gastrostomy tube, which was promptly replaced. She was sent back to her skilled nursing facility the same day and was pronounced deceased at her facility 6 days later.
Discussion
Stated capacity refers to a patient who meets the capacity criteria by verbalizing a choice after accounting for the risks, benefits, and alternatives while rationally manipulating the information. Medical beneficence is equated with minimizing risk and maximizing longevity, and in this framework, any treatment escalation even if futile may seem rational. The term demonstrated capacity refers to the continuity between a patient’s verbalized thought process and their actions or behaviors. For cases in which stated capacity and demonstrated capacity are misaligned, we first identify the patient’s wishes and overall care goals to develop a congruent treatment plan by talking to family, clinicians, or others involved in the patient’s care on a consistent basis. It is important that the patient has a rudimentary understanding of realistic treatment outcomes. Second, multidisciplinary discussions are needed to reach a consensus on decision-making capacity and to reduce bias on current capacity determination based on previous actions and behaviors. Finally, there should be a low threshold for ethics committees to become involved (Figure 1).
Conclusion
This case highlights a patient with a protracted history of contradictory behaviors to their verbalized treatment goals. It is important to consider the patient’s long-held values and actions while doing capacity assessments. This case emphasizes the importance of comprehensive and broad input from family and all treatment teams and the value of ethics committee consult. Realignment of treatment goals in the context of a patient’s global health state is important to reduce unnecessary patient suffering.
Article Information
Published Online: September 10, 2024. https://doi.org/10.4088/PCC.24cr03749
© 2024 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2024;26(5):24cr03749
Submitted: March 24, 2024; accepted May 28, 2024.
To Cite: Noe G, Gaba A, Munjal S. Stated versus demonstrated decision-making capacity how to approach this ethical conundrum. Prim Care Companion CNS Disord. 2024;26(5):24cr03749.
Author Affiliations: Wake Forest University School of Medicine, Winston-Salem, North Carolina (Noe, Gaba); Department of Psychiatry and Behavioral Medicine, Wake Forest University School of Medicine, Winston-Salem, North Carolina (Munjal).
Dr Noe is a first author, and Dr Munjal is a senior author.
Corresponding Author: Greg Noe, MD, Wake Forest School of Medicine, 1 Medical Center Blvd, Winston-Salem, NC 27103 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Publication consent was received from the patient and the patient’s sister (power of attorney). Information has been de-identified to protect anonymity.
References (3)

- Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment. N Engl J Med. 1988;319(25):1635–1638. PubMed CrossRef
- Appel JM. A values-based approach to capacity assessment. J Leg Med. 2022;42(1–2):53–65. PubMed CrossRef
- Owen GS, Freyenhagen F, Martin W. Authenticity, insight, and impaired decision-making capacity in acquired brain injury. Philosophy, Psychiatry Psychol. 2018;25(1):29–32.
Enjoy this premium PDF as part of your membership benefits!