Graves’ disease, an expression of an autoimmune process, is the most common cause of hyperthyroidism.1 It can be associated with various psychiatric symptoms, including in thyrotoxic patients with associated psychosis (thyrotoxic psychosis [TP]).2 TP is not a specific clinical picture, but affective psychoses tend to be the most common phenotype. Interestingly, the prevalence of mania/lifetime bipolar disorder is reportedly more frequent in both euthyroid and hyperthyroid women with Graves’ disease compared to women with no past or present thyroid disease.1
We present the case of a patient with a 2-year history of Graves’ disease, nonadherent to antithyroid treatment, who developed TP (mania with psychosis) and responded to antithyroid with adjunctive antipsychotic treatment, although, even after nonadherence to the latter, her symptoms of TP ultimately remitted.
Case Report
The patient was a 31-year-old woman with a 2-year history of Graves’ disease who presented to the emergency department (ED) by family for “bizarre behavior.” The patient’s history was notable for palpitations, tremor, increased stool frequency, thirst, polyuria, and amenorrhea of unknown duration. Furthermore, the patient had been nonadherent for an unknown period to methimazole. The physical examination was significant for tachycardia (pulse = 181 bpm), systolic hypertension (190/91 mm Hg), fine tremor, hyperkinesis, mild proptosis, and palpable goiter. The neurologic examination was unremarkable. As a result, the patient was admitted to the general medicine service, and we were consulted for “change in her behavior.”
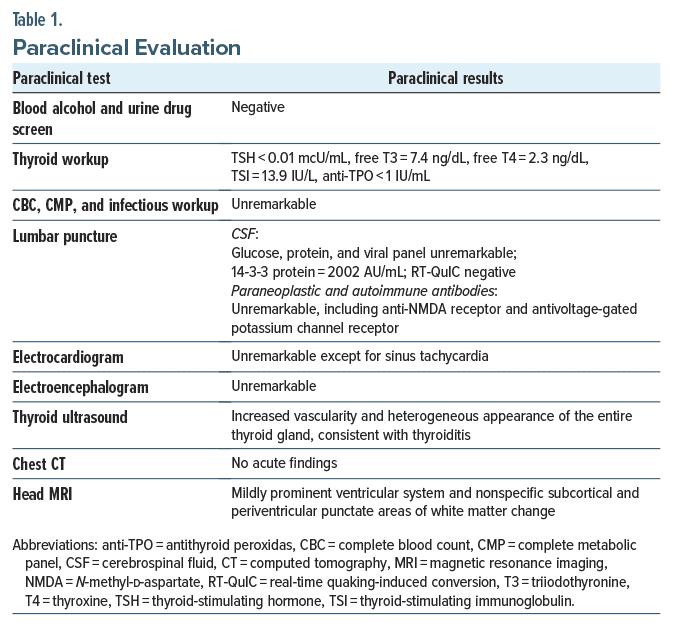
On evaluation, the patient demonstrated an elated mood with increase in energy. Her speech was pressured with flight of ideas. Notably, the patient had both grandiose and paranoid delusions. According to the family, she developed these manic symptoms 1 day prior to this admission. The patient was not taking psychotropic medications, although 6 months earlier, the patient presented with similar phenomenology in the context of nonadherence to methimazole. During the previous admission, she was stabilized on methimazole and adjunctive olanzapine; however, due to leukopenia, olanzapine was discontinued, and aripiprazole 5 mg/d was substituted. She was nonadherent to aripiprazole after discharge from this prior admission. The patient’s Young Mania Rating Scale (YMRS)3 score was 38. She had no personal or family psychiatric or substance abuse history. As mentioned, the patient had been reportedly nonadherent to methimazole. Table 1 provides the patient’s paraclinical evaluation.
The patient began a course of methimazole (10 mg/d), propranolol (20 mg every 6 hours), and aripiprazole (5 mg/d, increased to 15 mg/d after 2 days). After 2, 4, and 6 days of methimazole, propranolol, and aripiprazole 15 mg/d, she had YMRS scores of 34, 29, and 12, respectively. At that time, our patient’s vital signs were stable. She denied any symptoms that brought her to the ED, with a physical examination that was within normal limits. The patient was discharged on methimazole 10 mg/d and aripiprazole 15 mg/d. As the patient was normotensive, the primary team elected to discontinue propranolol at discharge. One month after discharge, the patient presented to endocrinology and had reportedly been nonadherent to aripiprazole. At this appointment, she had a thyroid-stimulating hormone (TSH) level of 0.09 mcU/mL, and both triiodothyronine (T3) and thyroxine (T4) levels were within normal limits. Despite nonadherence to aripiprazole and methimazole, her YMRS score was 0.
Discussion
While a review of the pathogenesis of Graves’ disease is beyond the scope of this report, activating autoantibodies of the IgG1 subclass that are directed against the thyrotropin receptor are both specific for and central to Graves’ disease.4 Thyroid function appears to influence the course of affective disorders. For instance, excess mobilization of thyroid hormones reportedly increases the risk of mania in vulnerable individuals. Although other mechanisms may be involved,5 evidence suggests that the modulation of the β-adrenergic receptor (B-Ar) by thyroid hormones may accentuate the B-Ar’s response to catecholamines.6 Nonetheless, in some,7 but not all,8 studies, the correlation between mania/psychosis due to hyperthyroidism is supported. Others report TP is rare, and probands either have a premorbid history of bipolar disorder or genetic loading, such as a strong family history of bipolar disorder.7
While definitive treatment of TP in Graves’ disease is achieved with medical/surgical intervention on the underlying thyroidopathy,9 psychopharmacologic intervention should be considered when psychiatric symptoms are severe or treatment of the underlying condition alone does not lead to rapid improvement in the patient’s mental state.10 Thus, as initiated in our patient’s case and supported by previous reviews of case series, antithyroid drugs (ie, methimazole) combined with β-blockers (ie, propranolol) are the treatments of choice for hyperthyroidism presenting with psychotic symptoms.11
The severity of our patient’s mania (YMRS score = 38) warranted adjunctive antipsychotic treatment. While there is a dearth of controlled studies, in a review of treatment of psychosis in hyperthyroidism, there was no “gold standard” of treatment recommended. Thus, per the latter, we chose aripiprazole, a commonly utilized option that demonstrated relatively superior efficacy profiles of over 60%.9
Interestingly, on follow-up in the endocrinology clinic, our patient disclosed she was nonadherent to aripiprazole but adherent to methimazole. Notably, our patient was not manic/psychotic, yet paraclinical evidence of methimazole adherence included TSH level increasing to 0.09 mcU/mL, while both free T3 and T4 were within normal limits. Thus, while our case seems to offer support for first-line treatment of TP in Graves’ disease with methimazole and propranolol, the efficacy of acute adjunctive use of aripiprazole/ antipsychotics was not definitive. While our patient was adherent to aripiprazole for the 6 days of prescribed treatment during the hospitalization, there are only rare reports of adjunctive antipsychotics aiding in the treatment of TP for less than or equal to 6 days of therapy.9 Furthermore, despite nonadherence to aripiprazole after discharge from the hospital, our patient’s YMRS score continued to decrease to 0 and progressed towards euthyroidism.
In closing, while treatment of Graves’ disease, with or without TP, typically responds to antithyroid medications/β-blockers,12 adjunctive aripiprazole/another antipsychotic has been utilized based on the severity of TP. While our case potentially strengthens the evidence of antithyroid medications/β-blockers for the treatment of TP, it only offers equivocal support for adjunctive aripiprazole/ another antipsychotic. Nonetheless, we recommend that larger randomized controlled studies should be performed to further delineate a treatment algorithm for TP.
Article Information
Published Online: February 27, 2025. https://doi.org/10.4088/PCC.24cr03840
© 2025 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2025;27(1):24cr03840
Submitted: August 27, 2024; accepted December 2, 2024.
To Cite: Spiegel DR, Pilc E, Coleman T, et al. Thyrotoxic psychosis in a patient with Graves’ disease and methimazole nonadherence: the role of antipsychotics in treatment. Prim Care Companion CNS Disord. 2025;27(1):24cr03840.
Author Affiliations: Department of Psychiatry and Behavioral Sciences, Virginia Health Sciences/Eastern Virginia Medical School at Old Dominion University, Norfolk, Virginia (all authors).
Corresponding Author: David R. Spiegel, MD, Department of Psychiatry and Behavior Sciences, Eastern Virginia Medical School, 825 Fairfax Ave, Norfolk, Virginia 23507 ([email protected]).
Relevant Financial Relationships: Dr Spiegel is in the speaker’s bureau for Allergen, Alkermes, Otsuka, and IntraCellular but has no conflict of interest in preparation of this manuscript. The other authors have no disclaimer/ conflict of interest to report.
Funding/Support: None.
Patient Consent: Consent was verbally received from the patient to publish the case report, and information has been de-identified to protect anonymity.
References (12)

- Bunevicius R, Velickiene D, Prange AJ, Jr. Mood and anxiety disorders in women with treated hyperthyroidism and ophthalmopathy caused by Graves’ disease. Gen Hosp Psychiatry. 2005;27(2):133–139.
- Brownlie BE, Rae AM, Walshe JW, et al. Psychoses associated with thyrotoxicosis - ‘thyrotoxic psychosis.’ A report of 18 cases, with statistical analysis of incidence. Eur J Endocrinol. 2000;142(5):438–444.
- Young RC, Biggs JT, Ziegler VE, et al. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–435. PubMed
- Smith TJ, Hegedüs L. Graves’ disease. N Engl J Med. 2016;375(16):1552–1565. PubMed
- Häfner S, Schölch D. Graves’ disease and psychosis in a young woman: pathophysiologic considerations. Prim Care Companion CNS Disord. 2017;19(4):16l02081. PubMed
- Whybrow PC, Prange AJ. A hypothesis of thyroid catecholamine-receptor interaction: its relevance to affective illness. Arch Gen Psychiatry. 1981;38(1):106–113.
- Bunevicius R, Prange AJ. Psychiatric manifestations of Graves’ hyperthyroidism: pathophysiology and treatment options. CNS Drugs. 2006;20(11):897–909.
- Placidi GP, Boldrini M, Patronelli A, et al. Prevalence of psychiatric disorders in thyroid diseased patients. Neuropsychobiology. 1998;38(4):222–225.
- Golub D, Rodack V. Antipsychotics in hyperthyroid-related psychosis: case report and systematic review. Neuroendocrinol Lett. 2018;39(1):65–74.
- Hazen EP, Sherry NA, Parangi S, et al. Case 10- 2015: a 15-year-old girl with Graves’ disease and psychotic symptoms. N Engl J Med. 2015;372(13):1250–1258. PubMed
- Bennett B, Mansingh A, Fenton C, et al. Graves’ disease presenting with hypomania and paranoia to the acute psychiatry service. BMJ Case Rep. 2021;14(2):e236089. PubMed
- Adiba A. Association of thyrotoxicosis with mania. Am J Psychiatry Resid J. 2019;14:2–11.
Enjoy this premium PDF as part of your membership benefits!