The prevalence of substance use disorders is increased in schizophrenia1 and radically impacts its presentation, making the distinction between “primary” schizophrenia and substance-induced psychosis uncertain.2 According to the “primary addiction hypothesis,” the dysfunction in the reward dopaminergic system in schizophrenia could favor the use of substances of abuse modulating its activity. The “self-medication hypothesis” proposes that stimulants and caffeine can be sought to counteract negative symptoms, sedation, fatigue, and cognitive fog primary or secondary to antipsychotics.3 Recently, sugar was established as a potential substance of abuse due to the release of dopamine and endogenous opioids.4
Cola combines the effects of caffeine and sugar, which could be multiplicative; however, while there are clues that a cola use disorder could exist in the general population,5,6 in the psychiatric population it was clinically described only once in a woman with major depression.7 The present case describes a transient cola addiction, lasting around 6 months, in a patient with schizophrenia.
Case Report
Mr A had a 27-year history of schizophrenia, with multiple acute psychotic episodes characterized by behavioral disorganization, auditory verbal hallucinations, and paranoid delusions, requiring 12 admissions in a psychiatric hospital. He was known to have tobacco and sporadic cannabis use, but not other addictions. At the material time, he had been well stabilized for several months, with only slight residual symptoms in the form of suspiciousness, bizarreness, amotivation, and blunted affect. He was regularly attending his psychiatric consultations and accepted monotherapy with long-acting injectable paliperidone 150 mg/ month. Over several weeks, with no clear provocative factor, he progressively increased his intake of cola, driven by an inexplicable craving; even if able to recognize the consumption as excessive, he was not worried or trying to cut down his use, remaining in a precontemplative stance.
The phenomenology met the criteria for a substance use disorder: an irresistible need to experiment the pleasurable effect of cola, tolerance leading to increasing intake, withdrawal symptoms in the form of headache and fatigue, and spending a large amount of the day seeking, consuming, or recovering from the effects of cola. Throughout this time, his habits changed: an impulsive phase characterized by lack of meditation, urgency, and sensation seeking was followed by a routine consumption without a clear pleasurable effect, more in line with a compulsive modality.
Motivational dialogue was used as a therapeutic strategy, with no measurable effect; the maximum consumption reached an estimate of 5 L/d. At the same time, a low plasma level of paliperidone was detected, which previously had always been within normal limits; our interpretation relied on an exalted renal clearance of the medication due to the increased water intake and the diuretic effect of caffeine and glycosuria. After several weeks, the overuse gradually decreased spontaneously until resolution; during the whole episode, no signs of psychotic decompensation emerged.
Discussion
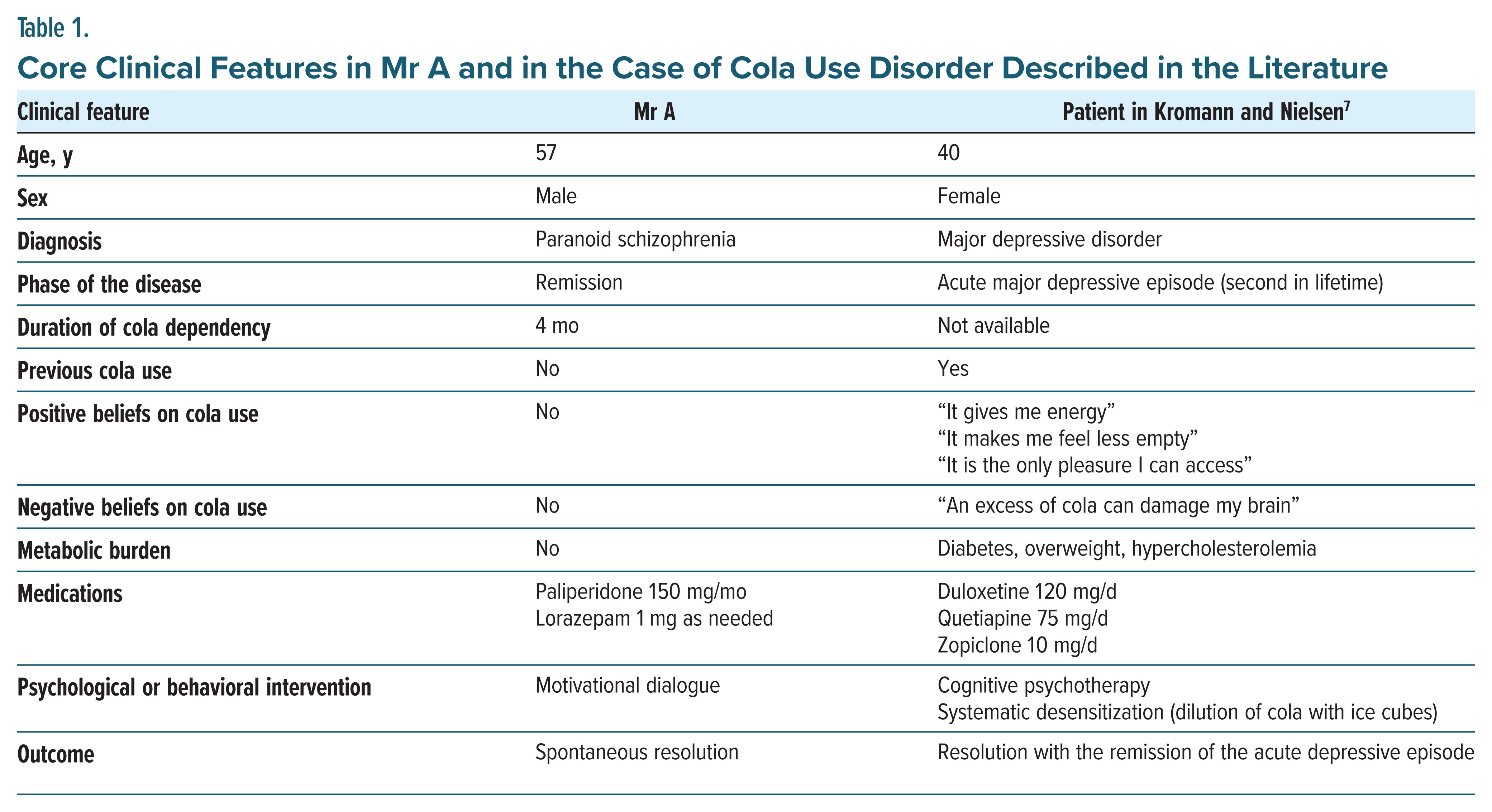
Substance use disorders are common in schizophrenia, but to my knowledge, a consumption of cola meeting the criteria for a substance use disorder was never described. While typical for the succession of an impulsive phase and a compulsive phase, the course was peculiar for the scarce mentalization, for the nonattribution of meaning to the consumption, and for the sudden and inexplicable onset and end of the disorder. Table 1 describes Mr A’s main clinical features and those of the other previous case of cola dependency in the literature.7
Cola dependency is potentially linked to metabolic syndrome due to sugar content and to hyponatremia due to the increased water intake, issues that were not observed in Mr A. However, cola intake was interpreted as responsible for an increased renal clearance of paliperidone, exposing the patient to a risk of psychotic relapse due to ineffective dosing.
Article Information
Published Online: September 12, 2024. https://doi.org/10.4088/PCC.24cr03765
© 2024 Physicians Postgraduate Press, Inc. Prim Care Companion CNS Disord 2024;26(5):24cr03765
Submitted: May 5, 2024; accepted July 16, 2024.
To Cite: De Pieri M. Transient cola use disorder in a patient with schizophrenia.
Prim Care Companion CNS Disord. 2024;26(5):24cr03765.
Author Affiliation: Division of Adult Psychiatry, Department of Psychiatry, Geneva University Hospitals, Thônex, Switzerland.
Corresponding Author: Marco De Pieri, MD, PhD, Division of Adult Psychiatry, Department of Psychiatry, Geneva University Hospitals, Chemin du Petit-Bel-Air 2, CH 1226 Thônex, Switzerland ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: The patient provided written consent to publish this case report, and information has been de identified to protect anonymity.
References (7)

- Hunt GE, Large MM, Cleary M, et al. Prevalence of comorbid substance use in schizophrenia spectrum disorders in community and clinical settings, 1990–2017: systematic review and meta-analysis. Drug Alcohol Depend. 2018;191:234–258. PubMed CrossRef
- Fiorentini A, Cantù F, Crisanti C, et al. Substance induced psychoses: an updated literature review. Front Psychiatry. 2021;12:694863. PubMed CrossRef
- Khokhar JY, Dwiel LL, Henricks A, et al. The link between schizophrenia and substance use disorder: a unifying hypothesis. Schizophr Res. 2018;194:78–85. PubMed CrossRef
- Avena NM, Rada P, Hoebel BG. Evidence for sugar addiction: behavioral and neurochemical effects of intermittent, excessive sugar intake. Neurosci Biobehav Rev. 2008;32(1):20–39. PubMed CrossRef
- Campos-Ramírez C, Camacho-Calderon N, Villagran Herrera ME, et al. Soft Drink Addiction Scale: reliability and validity analysis in young Mexican people. Beverages. 2024;10(1):15.
- Falbe J, Thompson HR, Patel A, et al. Potentially addictive properties of sugar-sweetened beverages among adolescents. Appetite. 2019;133:130–137. PubMed CrossRef
- Kromann CB, Nielsen CT. A case of cola dependency in a woman with recurrent depression. BMC Res Notes. 2012;5(1):692. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!