Trichotillomania, or hair-pulling disorder, is a common psychiatric condition characterized by persistent, uncontrollable urges to remove hair from various parts of the body. This behavior usually follows a stress inducing situation, thus causing impairment to function in day-to-day activities.
Trichotillomania affects between 0.5% and 2.0% of people over the course of their lifetimes.1 The signs of this disorder include constantly pulling out hair, breaking off sections, eating or storing hair, and feeling comforted after pulling hair. Major depressive disorder and anxiety disorder are commonly associated with this condition.
One of the most often used behavioral strategies for the treatment of trichotillomania is habit reversal therapy (HRT), which comprises awareness training, self-monitoring, and competing response.2 Patients conventionally undergo this therapy on an outpatient or inpatient basis. Lockdowns imposed due to the COVID-19 pandemic made it difficult to conduct therapy in these conventional settings; thus, health care providers and patients had to find alternative methods for conducting and continuing treatment. There was an emergence of tele-based therapy during that time, and it had successful results for many psychiatric conditions.3
Over the last 2 decades, tele-based psychotherapeutic interventions have steadily gained importance and acceptance. Teletherapy includes psychological services offered via phone, computer, or video conferencing platforms and has been shown to be successful in treating trauma, depression, and other mental health conditions among diverse populations. A retrospective longitudinal study4 using online video teletherapy for the treatment of obsessive-compulsive disorder (OCD) found a 43.4% mean reduction in obsessive-compulsive symptoms and a 62.9% response rate. Treatment also resulted in a 44.2%, 47.8%, and 37.3% mean reduction in depression, anxiety, and stress symptoms, respectively. Improvements were maintained at 3, 6, 9, and 12 months. The video teletherapy treatment used in that study4 demonstrated effectiveness in reducing symptoms and improved quality of life as well. We present a case of trichotillomania in a patient who was managed through telepsychiatry-based HRT during the COVID-19 pandemic.
Case Report
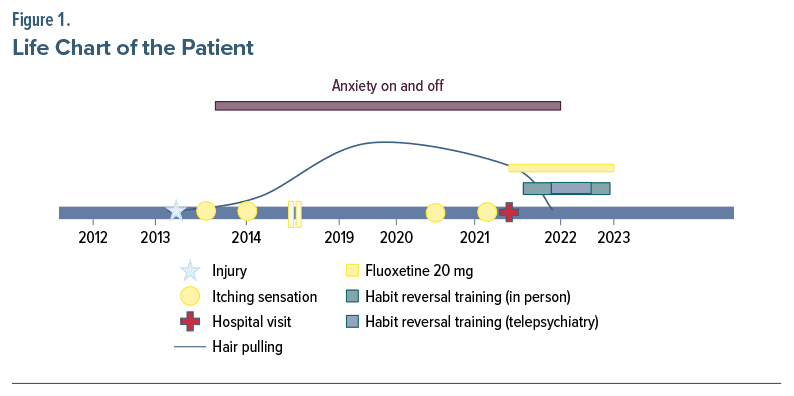
The patient was a 19-year-old single female 12th pass student and resident of a village in North India, with uneventful prenatal, natal, and postnatal events and normal development. While playing at age 11 years, she had an injury followed by scarring at the back of her scalp. Following conservative management for the injury, she gradually over a 1-year period started having symptoms characterized by an itching sensation followed by pulling of hair from the same site at age 12. These symptoms had an insidious onset and a continuous and rogressive course (Figure 1). The pattern of pulling was by rolling and pulling hair close to the roots. Frequency of hair pulling was 30–40 hairs per day and sometimes in stressful situations reached up to 50–60 hairs. She spent almost 3–4 hours per day pulling hair. After pulling the hair, she separated the roots from the rest of the hair and threw it away. Since the hair pulling gradually became generalized, it caused visible patches of baldness. She started avoiding going out and when she had to would mostly part her hair sideways or cover the scalp with a scarf. At the same time, she complained of restlessness whenever she saw the broken hairs, which impaired her concentration and performance on a mock examination.
Due to increasing baldness, family members took her to a dermatologist. She was prescribed serum and medication (details not available), but given non-improvement and the specific hair loss pattern, she was referred for psychiatric evaluation. She presented to our outpatient services and was diagnosed with trichotillomania per ICD-10 criteria. She was started on fluoxetine 20 mg for the trichotillomania and comorbid anxiety symptoms. She was psychoeducated about trichotillomania, and the need for HRT was explained. As a part of HRT, awareness training was started, and she was asked to keep a record of triggers, urges, and consequences of hair pulling and to collect the hair in a ziplock bag. Ratings were done using the Psychiatric Institute Trichotillomania Scale5 (score of 30) and the Massachusetts General Hospital Hair Pulling Scale6 (score of 20). She was continued on medication and was taught the Jacobson progressive muscle relaxation exercise.7 Further, stimulus control and competing responses were also taught as part of therapy.
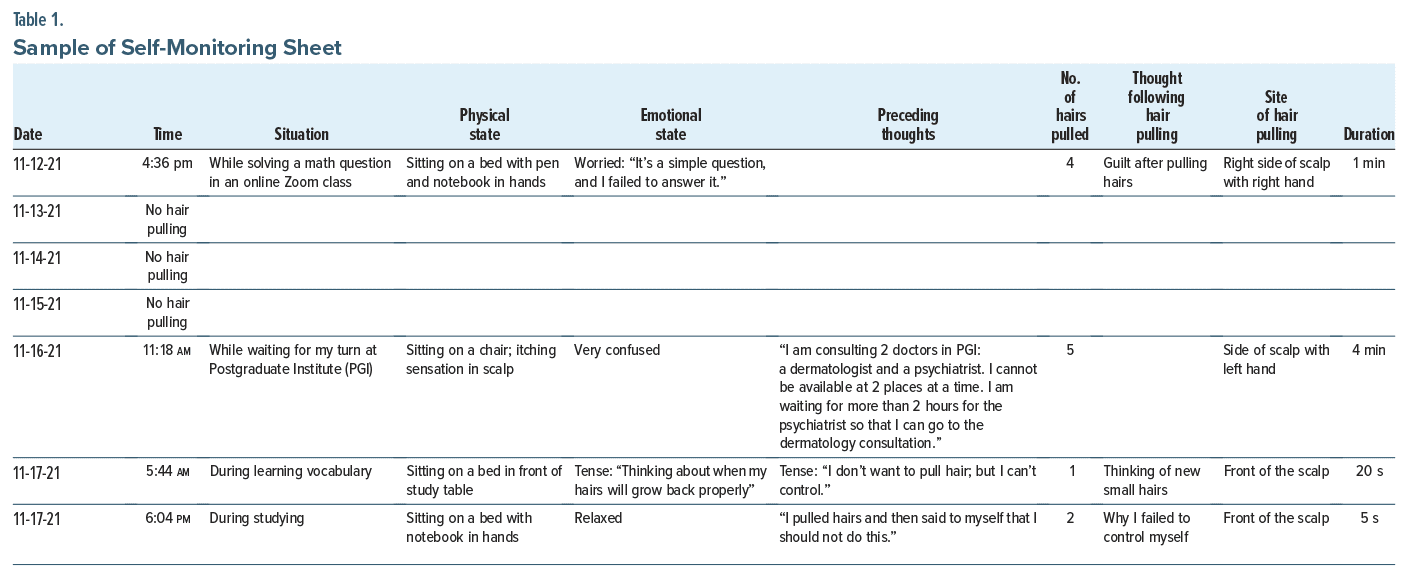
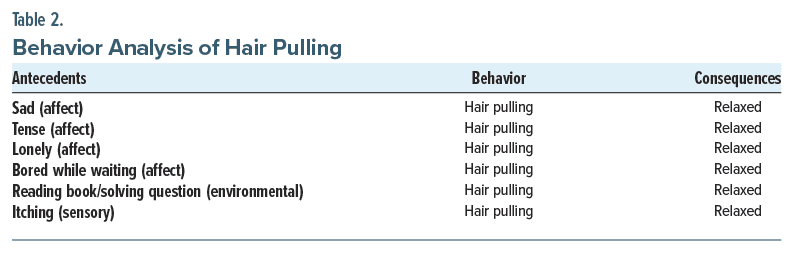
Due to a surge of a second wave of COVID-19 in the latter half of 2021, outpatient department patients were attached to telepsychiatry services by mid-November 2021. After discussion of the change in treatment modality, we planned for 2 weekly follow-ups via telepsychiatry (through the Zoom platform) with self-monitoring through Google Sheets (Table 1) and gave access to the patient, asking her to update every day. Behavioral analysis was also done during that time (Table 2). In the beginning, we faced issues of poor connectivity and missed timings of consultation while planning the sessions. But after 2 to 3 consultations, both parties got used to the change in modality of treatment and maintained the consensus throughout. This made it easier to continue with the treatment and therapy without coming to the clinic for physical follow-ups and therapy sessions. The doctor would go through the Google Sheets daily and give feedback, such as “Good job, keep it up,” on a regular basis to keep the patient motivated.
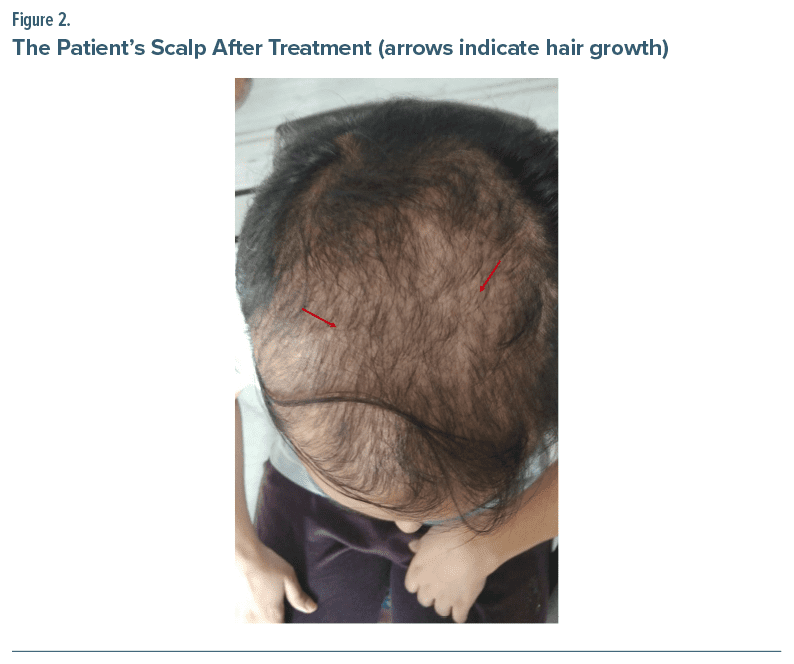
Within the first week of December 2021, her hair pulling reduced to 1 to 2 hairs per day. Other steps of HRT and relaxation exercise were continued as before. Tele-based therapy sessions were taken monthly thereafter, and by May 2022, she passed her college entrance exam and shifted to another city for studies Since outpatient department services had resumed, the patient came for follow-up before going to college. She reported no hair pulling, and her anxiety symptoms had reduced. By this time, the Psychiatric Institute Trichotillomania Scale score was 4, and the Massachusetts General Hospital Hair Pulling Scale score was 2. At subsequent follow-ups, the patient was continued on fluoxetine 20 mg with self-monitoring. She was not on dermatology treatment at that time. Her last follow-up was in January 2023, during which she was found to be maintaining well with new hair growth on the scalp (Figure 2) (pretreatment photo of the scalp is not available).
Discussion
Trichotillomania is a condition marked by compulsive hair pulling induced by stress. A variety of affective states can elicit hair pulling, which can help alleviate distress. As reported in the literature, anxiety has frequently been attributed to the majority of the functional impairment associated with trichotillomania.8 The present case illustrates how trichotillomania with concomitant anxiety can present to psychiatry outpatient services.
The patient’s worry over her studies was a major contributing factor in her hair-pulling behavior. In the latter part of her illness, she started having worries due to her increasing baldness, thus worsening her anxiety and leading to more hair pulling, which caused her to maintain a vicious cycle. Such issues can be seen in other psychiatric conditions like OCD, phobia, and panic disorder.8
Dermatologists can diagnose this condition earlier, as most people present to them due to concerns of hair loss and visible baldness as seen in our patient. If any unusual pattern of hair loss is noted or if there is a history of psychiatric illness in the past, it warrants a timely referral to a psychiatrist by any medical professional.
HRT is an effective behavioral therapy for trichotillomania.2 After providing psychoeducation about the therapy, the patient in our case was motivated to continue HRT, but due to the COVID-19 lockdown and shutting down of the outpatient services, we had to plan for continuation of treatment through telepsychiatry services. At that time, only a few tele-based treatments had been studied for disorders like agoraphobia, chronic tinnitus, and hoarding disorder.9
For trichotillomania, very few cases were reported using tele-based nonpharmacologic treatment. In one of the randomized controlled trials, participants in the tele-based treatment using acceptance and commitment therapy for trichotillomania reported significant improvement in hair-pulling symptoms, psychological flexibility, total distress, stress, and depression compared to the waitlist group.10 But the authors do mention that average quality of life did not improve. Many participants did see improvement, but limitations of the study were due to assessments and lost to follow-up.10
Tele-based treatment offers promising results and has clinical implications, including treatment accessibility across rural and urban areas without limitations, such as those imposed by the COVID-19 pandemic, or other barriers to providing quality care. However, there have been concerns that telepsychiatry can hinder conventional practice and create a false sense of “presence.” But some systematic reviews have found no significant difference in patient satisfaction with video conferencing as a modality to deliver mental health services compared to in person consultation.11
While we planned for the therapy via telepsychiatry, in the beginning we faced some issues as described in the literature. Since it was a newer modality of treatment, not many patients or even doctors were welcoming to its usage. Nevertheless, with repeated reassurance and constant feedback we gradually proceeded with this treatment.
Sometimes while planning for teleconsultation and therapy, we encounter issues of usage related to mobile phones, laptops, and internet connectivity among both parties. As our patient was quite motivated and technology savvy with regard to the use of a mobile phone and laptop, we did not face this challenge. After 1 to 2 sessions, she was comfortable while communicating via the teleconsultation and would update the Google Sheets almost every day.
Cognitive sophistication and an understanding of technology are important when planning such therapy; otherwise, the results will not be very fruitful. In addition, an issue of privacy does remain while conducting therapy. In the present case, we ensured that the patient was alone and that her privacy was respected from our side as well. Sometimes, such privacy issues can result in disruption of rapport and early dropouts.
The use of Google Sheets for self monitoring was tailored to meet the patient’s needs. The patient gave positive reviews on its use and indicated improvement in hair pulling while monitoring, and constant feedback from the doctor motivated her to reach her goal. The use of Google Sheets for the purpose of such therapy is, to our knowledge, the first of its kind, so this makes this case unique in terms of using innovative ways to conduct a therapy. When used with thorough supervision, monitoring sheets can also be used in the treatment of other common psychiatric conditions like OCD, anxiety disorders, and panic disorders. Nevertheless, issues with privacy and internet and technology accessibility remain. More studies in terms of meta-analysis and systematic review need to be done to establish the efficacy of Google Sheets for use in therapy. The present case illustrates how trichotillomania manifests and how it can be treated using tele based HRT.
Article Information
Published Online: January 7, 2025. https://doi.org/10.4088/PCC.24cr03785
© 2025 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2025;27(1):24cr03785
Submitted: June 4, 2024; accepted September 6, 2024.
To Cite: Rijal R, Adarsh H, Chauhan N. Innovative strands of healing: nurturing recovery in a case of trichotillomania via tele-based habit reversal therapy. Prim Care Companion CNS Disord. 2025;27(1):24cr03785.
Author Affiliations: Rhythm Neuropsychiatry Hospital and Research Centre, Ekantakuna, Kathmandu, Nepal, (Rijal); Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh, India (Adarsh, Chauhan).
Corresponding Author: Nidhi Chauhan, MD, DM, Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Nehru Hospital, Cobalt Block, Level III, Chandigarh, India ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Consent was received the patient’s legal guardian to publish the case report and photo. Information, including dates, has been de-identified to protect anonymity.
References (11)

- Grant JE. Trichotillomania (hair pulling disorder). Indian J Psychiatry. 2019;61(suppl 1):S136–S139. PubMed
- Gupta S, Gargi PD. Habit reversal training for trichotillomania. Int J Trichology. 2012;4(1):39–41. PubMed CrossRef
- Ibragimov K, Palma M, Keane G, et al. Shifting to tele mental health in humanitarian and crisis settings: an evaluation of Médecins Sans Frontières experience during the COVID-19 pandemic. Confl Health. 2022;16(1):6–5.
- Feusner JD, Farrell NR, Kreyling J, et al. Online video teletherapy treatment of obsessive-compulsive disorder using exposure and response prevention: clinical outcomes from a retrospective longitudinal observational study. J Med Internet Res. 2022;24(5):e36431. PubMed
- Winchel RM, Jones JS, Molcho A, et al. The Psychiatric Institute Trichotillomania Scale (PITS). Psychopharmacol Bull. 1992;28(4):463–476. PubMed
- Keuthen NJ, O’Sullivan RL, Ricciardi JN, et al. The Massachusetts General Hospital (MGH) Hairpulling Scale: 1. Development and factor analyses. Psychother Psychosom. 1995;64(3–4):141–145. PubMed CrossRef
- Mushtaq B, Ajaz Ahmad K. Jacobson muscle relaxatation technique (Jpmr) (20 Min). JOJ Nurs Health Care. 2018;8:755–757.
- Grant JE, Redden SA, Leppink EW, et al. Trichotillomania and co-occurring anxiety. Compr Psychiatry. 2017;72:1–5. PubMed CrossRef
- Ivanova E, Lindner P, Ly KH, et al. Guided and unguided acceptance and commitment therapy for social anxiety disorder and/or panic disorder provided via the internet and a smartphone application: a randomized controlled trial. J Anxiety Disord. 2016;44:27–35. PubMed CrossRef
- Lee EB, Haeger JA, Levin ME, et al. Telepsychotherapy for trichotillomania: a randomized controlled trial of ACT enhanced behavior therapy. J Obsessive Compuls Relat Disord. 2018;18:106–115.
- Malhotra S, Chakrabarti S, Shah R. Telepsychiatry: promise, potential, and challenges. Indian J Psychiatry. 2013;55(1):3–11. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!