The digital age has transformed our lives, impacting how we connect, work, and entertain ourselves, while raising concerns about mental health. Smartphones, social media, online gaming, and streaming platforms have reshaped information acquisition and social interaction, yet they also affect mental well-being. With an estimated 5.30 billion internet users globally, these challenges vary among individuals, particularly among those with preexisting conditions such as major depressive disorder (MDD), attention-deficit/hyperactivity disorder (ADHD), and generalized anxiety disorder (GAD).1–3 These conditions, affecting approximately 280 million people globally as of 2023, present unique struggles, compounded by the pervasive influence of digital technology.2,4
In the digital era, screen time has surged, with users spending an average of 6 hours and 41 minutes online daily.5 This increase in use underscores the omnipresence of digital technology and its potential repercussions, especially for those with mental health issues. We present the case of a 24-year-old woman battling MDD, ADHD, and GAD, conditions that severely hamper joy and concentration and induce excessive worry.4 Her decision to seek therapy through a digital deaddiction program highlights a troubling reality: the virtual world, often an escape, can exacerbate mental health issues.
In the recent era, several digital deaddiction programs have emerged as a response to the growing concerns surrounding excessive screen time and phone addiction. The emergence of new technologies presents both challenges and opportunities for mental health and well-being. However, it is essential to recognize that many of these programs lack the necessary credentials, regulation, and mental health expertise.
Our case emphasizes the importance of understanding the intricate relationship between excessive screen time, mental health, and the potential risks associated with digital deaddiction programs. Subsequent sections will delve into the patient’s challenges, the sequence of events, symptom management, and the journey toward recovery, aiming to underscore the importance of vigilant care in such cases.
Case Report
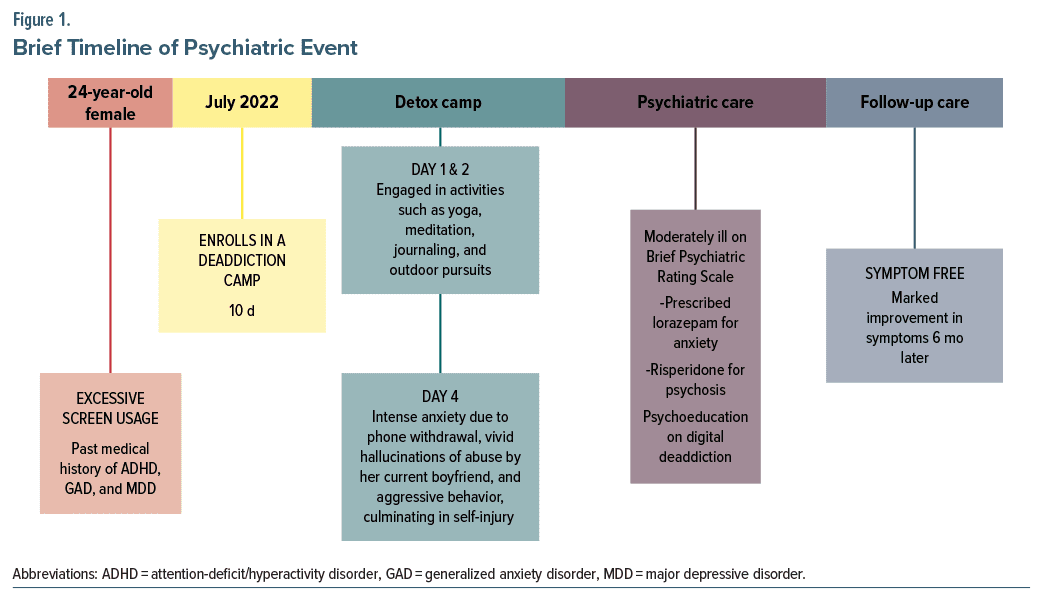
A 24-year-old Indian woman with a history of MDD, ADHD, and GAD presented with ongoing auditory and visual hallucinations and aggressive behavior. These symptoms manifested while she was undergoing treatment at a digital deaddiction camp due to her 10-year history of excessive screen time usage, mainly involving social media, online gaming, and streaming platforms. This prolonged exposure to screens had led to low concentration, a short attention span, and heightened anxiety, as reported by the patient. Three years earlier, she had been diagnosed with MDD, characterized by a depressive episode following a breakup with her long-term partner. Her previous depressive episodes had been successfully managed with fluoxetine and psychotherapy, and she had not experienced a depressive episode in the past 2 years.
The patient had attended a 10-day digital detox camp in the mountains, accompanied by a childhood friend. The luxurious camp permitted limited digital access, encouraging participants to engage in beneficial activities such as yoga, meditation, journaling, and outdoor pursuits. Daily activities started at 8:00 AM every morning and ended by 4:00 PM. However, on the second and third days, the patient experienced heightened anxiety due to abrupt digital withdrawal.
By the fourth day, her anxiety intensified, leading to vivid hallucinations of abuse by her current boyfriend and aggressive behavior, culminating in self-injury. Despite immediate first aid and evaluation at a clinic, the patient and her caregiver hesitated to seek psychiatric care due to concerns about stigma and hospitalization. They also refused referral to a specialist, citing the significant mental toll it would take on the patient and her discomfort with being seen by another health professional in her current mental state, possibly, due to societal stigma, as her father was a well-known businessman in the community. The patient reported no previous incidents of psychotic episodes. The caregiver stated that the patient was behaving normally until day 4 of the program when she felt triggered by a conversation her peers were having about missing their partners. This triggered her to isolate herself in her room, and the other participants only became aware of a disruption in her mental state when they heard the window shattering. The patient had a single shallow bleeding cut on her hand, which was cleaned and rebandaged. The patient’s mental status examination revealed disorganized thoughts, severe distress, and physical symptoms indicative of acute psychiatric distress.
In the clinic, the Brief Psychiatric Rating Scale6 was employed, suggesting a rating of 48, falling within the moderately ill category. The patient’s mental status examination revealed disorganized thought processes, disorientation, and severe distress. Her vital signs included a pulse of 140 beats/minute, blood pressure of 136/74 mm Hg, and an elevated respiratory rate of 30 breaths/ minute. Her random blood glucose level fell within the normal range, and she had not experienced any recent changes in medication or diet over the past 8 months. She denied substance use, which was later verified by testing. There was no evidence of altered consciousness, pressured or fast speech, or recent sleep disturbance. The patient displayed hostility and easy irritability during the psychiatric interview. Her mood was depressed, and she exhibited an anxious and perplexed affect. Concentration was impaired, likely due to ongoing emotional flooding. Her height and weight were appropriate for her age, and her body mass index was in a healthy range. She reported disturbed sleep due to nightmares the previous 2 days but reported getting in 7 hours of sleep throughout the camp, which was normal for her.
Following evaluation, the patient responded positively to lorazepam for anxiety relief. Risperidone was initiated to manage psychotic symptoms, gradually tapering off over 6 months as symptoms resolved. Psychoeducation and individual and group therapy sessions focused on coping strategies, digital detoxification, and stress management. At the last follow-up, roughly 4 months after the episode, the patient’s psychiatric symptoms significantly improved, with no abnormalities noted in subsequent tests.
The patient was encouraged to seek specialist referral for ongoing psychiatric care in another city to address family concerns about stigma. No alterations were made to her medication regimen, and a structured digital use plan was established to promote healthier digital habits, emphasizing gradual reduction rather than complete cessation. The comprehensive management of the patient’s acute psychiatric symptoms, coupled with ongoing support and structured intervention, highlights the importance of tailored care in addressing the complex interplay between digital addiction and mental health (Figure 1).
Discussion
This case highlights the complexity of managing multiple psychiatric diagnoses, exacerbated by digital deaddiction. It serves as a cautionary tale, emphasizing the need to recognize the risks posed by digital deaddiction programs, especially for individuals with existing mental health conditions.
Digital-based solutions, such as web-based tools, mobile apps, wearables, and virtual reality platforms, have demonstrated effectiveness in assessing and treating various mental health issues, including depression, anxiety, and addiction. These programs are often marketed as mental health–boosting initiatives, promising liberation from the shackles of digital dependency. However, it is essential to recognize that many of these programs lack the necessary credentials, regulation, and mental health expertise. In our patient’s instance, a lack of experience with dealing with her psychosis exacerbated her mental state. Her refusal to be referred to a doctor or psychiatric facility also aggravated the problem, probably due to societal stigma and a lack of understanding of her disease. While the intentions of such programs are noble, their inadequacy in dealing with individuals susceptible to mental health issues becomes apparent when faced with real-world scenarios.7 Furthermore, digital deaddiction programs are not designed to deal with people who are prone to physical disorders, particularly psychiatric conditions like psychosis. These programs are often not run by mental health specialists and are frequently unregulated, making it difficult to manage people with underlying mental health difficulties. Their primary goal may be to reduce screen usage, but the implications for mental health are routinely disregarded. One of the major problems with digital deaddiction therapies is the lack of defined medical recommendations.
Stress-induced psychosis can occur because of the abrupt withdrawal from habitual digital activities during deaddiction programs, especially in individuals with a history of high screen time usage. This heightened stress can serve as a precipitating factor for the development of acute psychotic features, as observed in our case. This phenomenon, known as “first-time psychosis,” has been documented in individuals with predisposing factors and stressors.8 In our case, the patient’s susceptibility, combined with the sudden cessation of her digital coping mechanisms, created a perfect storm for the emergence of acute psychotic features.
Excessive screen time and phone phobia anxiety have become common in our digital age, aggravated by social media and phone addiction. The reported rates of internet addiction disorder vary, ranging from 0.3% to 38%.9 These differences can be attributed to differences in diagnostic criteria and assessment methods used across various countries. The review by Weinstein and Lejoyeux10 indicates that prevalence rates in the United States and Europe have been reported to fall between 1.5% and 8.2%, while other sources suggest rates ranging from 6% to 18.5%.11 Several cases of internet addiction disorder have been reported in the literature. The first documented case of psychotic symptoms during withdrawal from internet addiction was in 2012 by Mendhekar and Andrade.12 The authors12 concluded that internet addiction disorder is more likely a form of addiction than impulse control. Another case reported by Paik et al13 states that akin to substance abuse, individuals with internet addiction disorder show withdrawal symptoms, most typically mood or anxiety symptoms such as dysphoria, anxiety, irritability, and boredom. However, delusions, hallucinations, and withdrawal psychosis can also be seen in some vulnerable individuals, like the findings noted in our patient.13
When away from one’s phone, the thought of missing out on updates, notifications, or social interactions on social media platforms can heighten anxiety.14 Such behavior may perpetuate a cycle of anxiousness and screen dependency. This can be attributed to inherent neurobiological vulnerabilities in humans. Internet addiction has been shown to be associated with changes in the integrity of the brains’ white matter.15 Surfing the internet results in the release of dopamine in the nucleus accumbens,16,17 the reward center of the brain implicated in other forms of addiction.18 With continued exposure, the receptors in this area may become desensitized, resulting in tolerance and an increased need for more stimulation to achieve the same “high,” driving distinctive behavioral patterns aimed at avoiding withdrawal symptoms. Users of digital technology encounter multiple layers of gratification from various applications, with the internet using a variable ratio reinforcement schedule, like gambling.19 Regardless of the specific application, such as web browsing, social media, and video games, these activities employ unpredictable and variable systems of reward, and the experience of gratification is heightened when coupled with mood elevating or stimulating content.
Although technology addiction is not formally recognized by the DSM-5, it is acknowledged as a growing global concern. It is worthwhile to note that in 2013, the American Psychiatric Association included “internet gaming disorder,” which includes both online and offline gaming, in the DSM-5 with an emphasis on the need for further research.18
Impact on Gen Z. In a 2021 study by Paulich and colleagues,20 it was observed that children and adolescents were spending more time on screens and electronic media than ever before, with 95% of American teenagers having access to smartphones. The research indicated that excessive screen time was linked to negative outcomes in the mental health, behavior, and academic performance of 9- and 10-year-old children.20 Young adults appear to be more susceptible to nomophobia, possibly due to their greater familiarity with modern technologies.21 Their early exposure to digital devices make them susceptible to digital addiction. The COVID-19 pandemic further exacerbated this issue, with more children becoming digital addicts. A meta-analysis spanning 31 countries revealed a global internet use disorder prevalence of 6.0% among individuals aged 12–41 years, with the Middle East having the highest prevalence.22 Another meta-analysis spanning 3 decades found a global prevalence of internet gaming disorder at 4.6% among adolescents aged 10–19 years. Data also indicated that younger age groups were more affected by internet use disorder.23 Digital addiction caused significant distress, functional impairments, and comorbid psychiatric disorders, including ADHD, depression, and anxiety. Lockdowns during the COVID 19 pandemic amplified the issue, particularly among children and young adolescents, intensifying cases of digital addiction.24 Some Japanese experts have described a condition called “Hikikomori syndrome,” which explains the psychopathology behind excessive internet use in adolescents and the subsequent psychosis upon withdrawal.25 The condition is characterized by young adolescents locked up in their bedrooms and isolated from the outside world, hooked up to their gadgets and refusing to communicate even with family, leading to social isolation, loss of interest in other activities, and the internet serving as an escape from dysphoric mood and functional impairment.25
Limitations
This case report has limitations. First, digital deaddiction camps are often not run by mental health specialists and are frequently unregulated; thus, we have limited insight into the activities at the camp. Second, the patient’s psychosis could have multifactorial triggers. A new environment could possibly deprive her quality of sleep and could also contribute to her symptoms. Also, a higher altitude could possibly alter her arterial blood gas levels and cause her symptoms.
Conclusion
Excessive screen time, phone phobia anxiety, and the emergence of digital deaddiction programs are shaping the landscape of mental health challenges in the digital age. Anxiety related to screen addiction can exacerbate preexisting mental health conditions, and abrupt digital detoxification can lead to stress induced psychosis in susceptible individuals. It is crucial to recognize that digital deaddiction programs, while well-intentioned, often lack the necessary expertise to address the complex needs of individuals with psychiatric conditions. There is an urgent need for the development of clear medical guidelines and regulations to ensure that individuals seeking help for screen addiction and mental health issues are provided with appropriate care. Our case underscores the importance of a nuanced understanding of the intricate relationship between excessive screen time, mental health, and the potential risks associated with digital deaddiction programs. It serves as a clarion call to both mental health professionals and society at large, urging a more nuanced understanding of the intricate relationship between digital technology and mental health.
Article Information
Published Online: October 1, 2024. https://doi.org/10.4088/PCC.24cr03748
© 2024 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2024;26(5):24cr03748
Submitted: March 24, 2024; accepted July 10, 2024.
To Cite: Ahuja J, Elavia Z. “Get off your phone”: withdrawal psychosis during a digital detoxification camp. Prim Care Companion CNS Disord. 2024;26(5):24cr03748.
Author Affiliations: Dr. Ahujas’ Pathology and Imaging Center, Dehradun, India (Ahuja); Dr. D.Y. Patil Medical College, Hospital & Research Centre, Pimpri, Pune (Elavia).
Corresponding Author: Zenia Elavia, MD, Dr. D.Y. Patil Medical College, Hospital & Research Center, Sant Tukaram Nagar, Pimpri, Pune 411018 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Written consent was obtained from the patient for the publication of this report, and information has been de-identified to protect anonymity.
References (25)

- Global Digital Overview. Digital around the world. 2023. Accessed November 5, 2023. https://datareportal.com/global-digital-overview
- Institute of Health Metrics and Evaluation. Global health data exchange (GHDx). Accessed March 4, 2023. https://vizhub.healthdata.org/gbd-results/
- Twenge JM, Campbell WK. Associations between screen time and lower psychological well-being among children and adolescents: evidence from a population based study. JAMA Pediatr. 2018;172(1):35–40. PubMed CrossRef
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
- Statista. Daily time spent on the internet worldwide. 2023. https://www.statista.com/statistics/238104/daily-internet-usage-worldwide/
- Hofmann AB, Schmid HM, Jabat M, et al. Utility and validity of the Brief Psychiatric Rating Scale (BPRS) as a transdiagnostic scale. Psychiatry Res. 2022;314:114659. PubMed CrossRef
- Ebert DD, Zarski AC, Christensen H, et al. Internet and computer-based cognitive behavioral therapy for anxiety and depression in youth: a meta-analysis of randomized controlled outcome trials. PLoS One. 2015;10(3):e0119895. PubMed CrossRef
- Fusar-Poli P, McGorry PD, Kane JM. Improving outcomes of first-episode psychosis: an overview. World Psychiatry. 2017;16(3):251–265. PubMed CrossRef
- Chakraborty K, Basu D, Kumar KGV. Internet addiction: consensus, controversies, and the way ahead. East Asian Archives Psychiatry. 2010;20(3):123–132. PubMed
- Weinstein A, Lejoyeux M. Internet addiction or excessive internet use. Am J Drug Alcohol Abuse. 2010;36(5):277–283. PubMed CrossRef
- Young KS, Nabuco de Abreu C. Internet Addiction: A Handbook and Guide to Evaluation and Treatment. John Wiley & Sons, Inc; 2011.
- Mendhekar DN, Andrade C. Emergence of psychotic symptoms during internet withdrawal. Psychiatry Clin Neurosci. 2012;66:163. PubMed CrossRef
- Paik A, Oh D, Kim D. A case of withdrawal psychosis from internet addiction disorder. Psychiatry Investig. 2014;11(2):207–209. PubMed CrossRef
- Elhai JD, Gallinari EF, Rozgonjuk D, et al. Feeling bad on Facebook: depression disclosures by college students on a social networking site. Depress Anxiety. 2011;28(6):447–455. PubMed
- Lin F, Zhou Y, Du Y, et al. Abnormal white matter integrity in adolescents with internet addiction disorder: a tract-based spatial statistics study. PLoS One. 2012;7(1):e30253. PubMed CrossRef
- Bai YM, Lin CC, Chen JY. Internet addiction disorder among clients of a virtual clinic. Psychiatr Serv. 2001; 52(10):1397. PubMed CrossRef
- Ko CH, Liu GC, Hsiao S, et al. Brain activities associated with gaming urge of online gaming addiction. J Psychiatr Res. 2009;43(7):739–747. PubMed CrossRef
- American Society of Addiction Medicine. Public policy statement: definition of addiction. 2011. Accessed August 21, 2011. https://www.asam.org/docs/default-source/public-policy-statements/1definition_of_addiction_long_4-11.pdf
- Ding K, Li H. Digital addiction intervention for children and adolescents: a scoping review. Int J Environ Res Public Health. 2023;20(6):4777. PubMed CrossRef
- Paulich KN, Ross JM, Lessem JM, et al. Screen time and early adolescent mental health, academic, and social outcomes in 9- and 10-year-old children: utilizing the Adolescent Brain Cognitive Development℠ (ABCD) Study. PLoS One. 2021;16(9):e0256591. PubMed CrossRef
- Notara V, Vagka E, Gnardellis C, et al. The emerging phenomenon of nomophobia in young adults: a systematic review study. Addict Health. 2021;13(2):120–136. PubMed CrossRef
- Cheng C, Li AYL. Internet addiction prevalence and quality of (real) life: a meta-analysis of 31 nations across seven world regions. Cyberpsychol Behav Soc Netw. 2014;17(12):755–760. PubMed CrossRef
- Fam JY. Prevalence of internet gaming disorder in adolescents: a meta-analysis across three decades. Scand J Psychol. 2018;59(5):524–531. PubMed CrossRef
- Gorowska M, Tokarska K, Zhou X, et al. Novel approaches for treating internet gaming disorder: a review of technology-based interventions. Compr Psychiatry. 2022;115:152312. PubMed CrossRef
- Stip E, Thibault A, Beauchamp-Chatel A, et al. Internet addiction, hikikomori syndrome, and the prodromal phase of psychosis. Front Psychiatry. 2016;7:6. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!